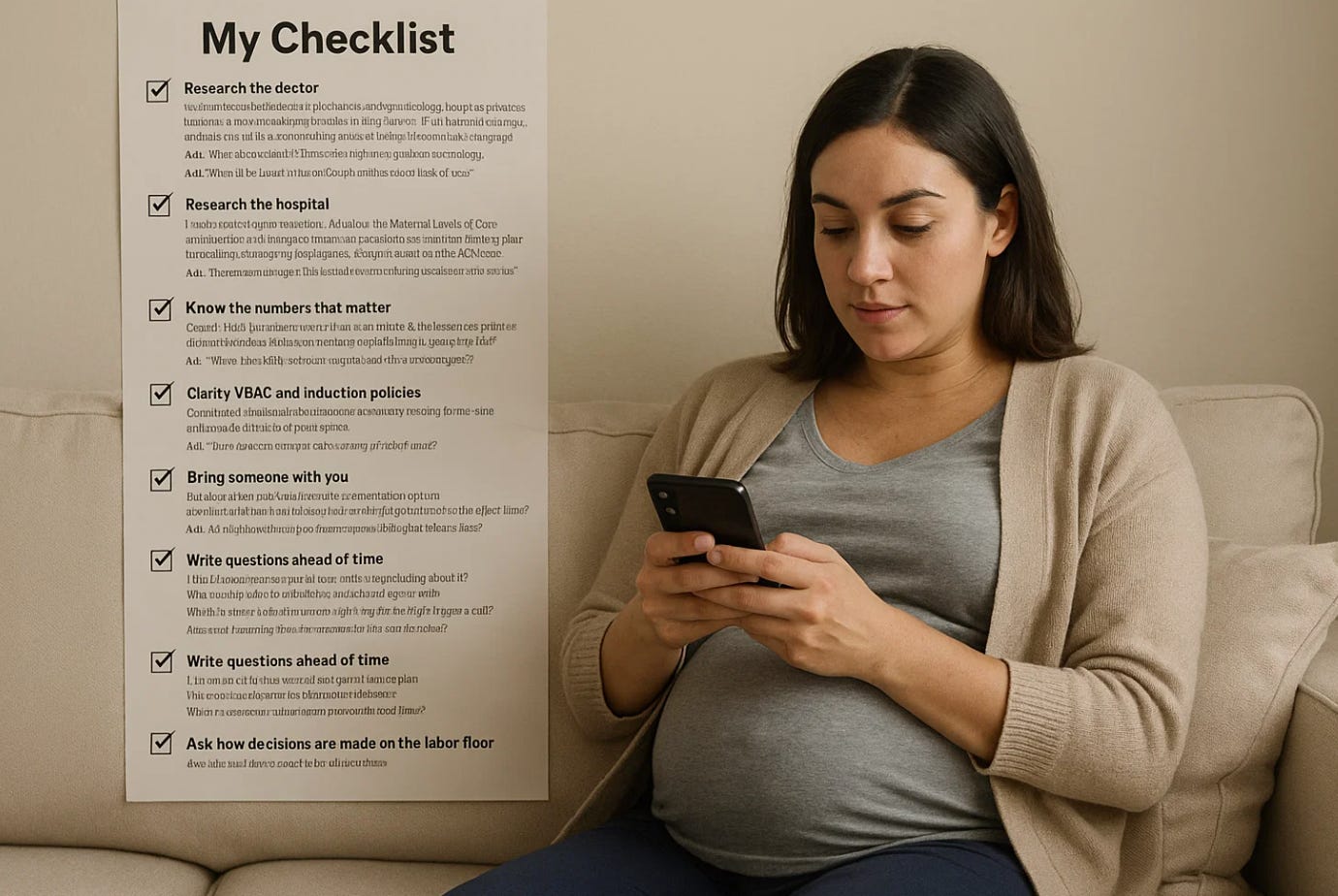
Your Pregnancy Safety Plan: 10 Moves That Put You in Control
The Safety Ledger: Most pregnancy problems are not about luck, they are about preparation. The safest births happen when patients and teams share a plan, speak up early, and write things down.
Here is a simple, practical guide to help you get the safest possible care.
Why this matters
As an obstetrician, a maternal-fetal medicine specialist, and an ethics professor, I have learned a clear lesson: safety grows from habits that anyone can learn. You do not need medical training to improve your odds. You need a plan, a partner, and a pencil, or a phone notes app. Safety is a team sport, and you are on the team.
In an emergency, seconds matter—and fumbling through paperwork or trying to remember critical details can cost precious time when you or your baby need help most. That’s why every pregnant woman should keep a comprehensive pregnancy safety file on her smartphone using a reliable, always-accessible app like iPhone Notes, Google Keep, or Samsung Notes. Think of it as your pregnancy command center: a single location containing your blood type, medication allergies, pregnancy complications, your obstetrician’s contact information, hospital preferences, and everything else that emergency responders, triage nurses, or covering physicians might need to know at 2 AM when your regular doctor isn’t available.
Copy/Paste Results
Make it a habit to regularly copy and paste lab results, ultrasound reports, doctor’s visit notes, and even screenshot or save images from your patient portal directly into this file—these records belong to you, and having your own complete copy ensures you’re never dependent on office hours, fax machines, or fragmented electronic health record systems when you need critical information.
Whether you’re traveling, switching providers, visiting the emergency department, or facing an unexpected complication, having this information instantly available on the device that’s always in your pocket transforms you from a passive patient into an active participant in your care. This isn’t about being anxious—it’s about being prepared. The ten essential moves outlined below will help you build this digital safety net in less than an hour, giving you the confidence that comes from knowing you’re ready for whatever your pregnancy journey brings.
1) Research the doctor
Look for board certification in obstetrics and gynecology, hospital privileges that match your needs, and a practice that offers 24/7 in-house coverage on the labor floor. Ask how often you will see your own doctor versus cross-coverage. Ask how the practice handles high-risk concerns and second opinions.
Ask: “Who will be there if I arrive at night, and how do you hand off care?”
2) Research the hospital
Hospitals are not all the same. Ask about the Maternal Levels of Care designation, which ranges from Level I to Level IV and describes staffing and resources for complex pregnancies. Many states and hospitals use the ACOG and SMFM framework. Some hospitals also pursue verification through The Joint Commission. Knowing the level tells you how ready the facility is if complications arise. pages.jointcommission.org+3ACOG+3ACOG+3
Ask: “What maternal care level is our hospital, and how does that affect my care if I develop a complication?”
3) Check for safety programs and “bundles”
Ask whether your hospital uses the AIM safety bundles for problems like severe hypertension and postpartum hemorrhage. These bundles are checklists of best practices that reduce preventable harm when used consistently.
Ask: “Do you use the AIM hemorrhage and hypertension bundles, and do you track results?”
4) Know the numbers that matter
Hospitals track quality measures. One key metric is PC-02: the low-risk first-time cesarean rate. Lower is usually safer when supported by good labor care. Ask what your hospital’s PC-02 rate is and how they work to improve it. The Joint Commission lists the Perinatal Care measure set that many certified programs use. Joint Commission+1
Ask: “What is our NTSV cesarean rate, and what steps are you taking to reduce unnecessary primary cesareans?”
5) Clarify VBAC and induction policies
If you had a prior cesarean, ask if TOLAC/VBAC is available and what criteria apply. ACOG supports VBAC in appropriate patients with immediate ability to perform an emergency cesarean if needed. For induction, ask how readiness is assessed and how much time is allowed before calling it a failed induction. ACOG notes that inductions, including elective 39-week inductions, often need generous time in early labor and adequate oxytocin trials.
Ask: “Do you offer VBAC, and what monitoring or staffing do you require to support it safely?”
6) Look for strong team communication
Safe labor units use briefs, huddles, and debriefs so everyone stays aligned as the situation changes. TeamSTEPPS, an AHRQ program, teaches these tools, and research links daily huddles to better safety culture. Ask how often the team huddles on Labor and Delivery and who leads those huddles.
Ask: “Do you hold regular L&D huddles, and how are decisions communicated to me and my support person?”
7) Bring someone with you
A second set of ears helps you remember details and lowers stress. Ask your support person to listen, take notes, and speak up if something seems unclear. If English is not your first language, ask for a certified medical interpreter. Clear language improves safety.
Ask: “Can my partner or support person be present during discussions and on rounds?”
8) Document your care in real time
Use your phone to build a simple documentation system:
Create a dedicated note with dates of each visit, medications, allergies, due date, and key plans.
Save photos or PDFs of ultrasounds, lab results, and the after-visit summary.
Record agreed next steps and what symptoms should trigger a call.
If your state allows it, ask before recording audio, then use voice memos for instructions.
Good notes turn confusion into clarity. They also help new team members catch up quickly.
Ask: “Can I get a printout or portal summary of today’s plan before I leave?”
9) Write questions ahead of time
Five targeted questions can change your care:
What is my main risk today, and what are we doing about it?
What are my options, with benefits and risks for each?
What signs mean I should call or come in right away?
If we do nothing today, what might happen?
When is my next check, and who is responsible for follow-up?
Bring the list to every visit and to triage. Check each box before you leave. Kep it on your smartphone in your saved notes.
10) Ask how decisions are made on the labor floor
Different units use different playbooks. Ask if the hospital uses written induction criteria, a shoulder dystocia drill schedule, and an emergency response plan for hemorrhage and blood bank release. Ask how fetal heart rate concerns are escalated, how residents and midwives coordinate with attending physicians, and how disagreements are resolved at the bedside. Units that teach and drill together perform better when seconds count. Many of these practices are part of standardized bundles and team training.
Ask: “If my labor plan needs to change, who will explain the options and document my consent in real time?”
A simple analogy
Think of your pregnancy like a cross-country flight. You choose an experienced pilot, a well-maintained aircraft, and an airline with a strong safety culture. You still buckle your seatbelt, listen to the safety briefing, and read the card. Safety comes from both the cockpit and the passenger seat. Health care is the same: your team needs to be excellent, and you need to be engaged.
What is new or overlooked
Patients often do not realize they can ask about hospital level of maternal care, safety bundles, and huddles. These are not private details, they are part of how a hospital shows its safety work. Knowing these basics helps you pick the right setting and ask sharper questions. It also makes it easier for your clinicians to partner with you when decisions change quickly.
Practical takeaways for your next visit
Bring a support person, a written question list, and one place to store notes and files.
Ask about maternal care level, AIM bundles, huddles, VBAC and induction policies, and your hospital’s PC-02 rate.
Before you leave, repeat back the plan: diagnosis, options, red flags, and next steps.
Use your patient portal and set reminders for tests, vaccines, and visits.
Reflection and ethical question
Safety is a shared duty. Clinicians owe you skill, transparency, and timely action. You owe yourself preparation, questions, and honest reporting of symptoms. Ask yourself: if I had to make a fast decision tonight, have I prepared the notes, the questions, and the support that would help me choose well? Share your plan in the comments, and let us learn from each other.