When the Strip Speaks in Two Languages: Why Generative AI Can Finally Help Us Read Fetal Monitoring Correctly
Obstetricians focus on the fetal heart rate. AI can restore what we have been missing all along: the uterus.
Cardiotocography (aka “fetal monitoring”) and the Promise We Forgot
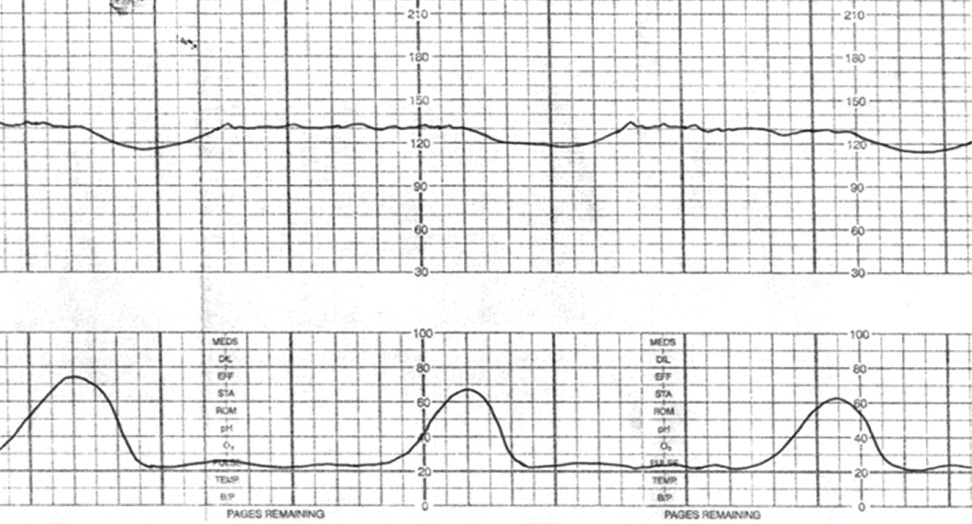
Cardiotocography, known simply as “fetal monitoring” in American labor wards, arrived in the 1960s with an elegant premise. Two sensors. Two tracings. One captured the fetal heart rate as an indicator of fetal wellbeing; the other recorded uterine contractions as the physiologic stressor. Together, they would reveal a conversation between mother and fetus that clinicians could read in real time.
The technology spread across labor and delivery units faster than the evidence supporting it. By the 1980s, continuous electronic fetal monitoring had become the standard of care in the United States, applied to over 85% of laboring patients today. The promise was explicit: this dual-channel window into the fetus-uterus relationship would identify compromise before it caused harm.
In November 2025 the New York Times calls it “the worst test in medicine”.
Seems something happened on the way to universal adoption. One signal came to dominate our attention, our charting, and our medicolegal consciousness. The other receded into visual noise.Fetal heart rate monitoring was designed as a dual-signal system: one line for the fetal heart rate and one line for uterine activity. Yet in modern practice, the tracing is often reduced to a single signal. What clinicians “see” and what they chart overwhelmingly centers on the fetus. The uterus, the source of the physiologic stress, becomes the background. This imbalance is not intentional. It is the predictable result of time pressure, cognitive overload, and an interface that visually favors the fetal heart rate. Generative AI can correct this. It can restore the physiologic relationship between the two signals and transform how we detect and manage fetal compromise.
Why this matters now
Labor units are overwhelmed. Inductions have become normal, labors have lengthened, comorbidities have risen, and fetal heart rate patterns have grown more complex. As staffing thins and workloads increase, clinicians must interpret hours of monitoring data in seconds. We know how often this results in delayed recognition of fetal stress, poorly titrated oxytocin, or confusion about deceleration types. Generative AI is finally capable of analyzing CTG signals in parallel, recognizing early patterns, explaining physiologic relationships, and reducing the background noise that clouds clinical decision-making.
The key insight is simple. Obstetricians tend to focus on the fetal heart rate because it is alarming, dynamic, and emotionally charged. But the uterus is the engine. Contraction quality, frequency, morphology, resting tone, and relaxation interval determine whether the fetus experiences adequate perfusion or progressive hypoxemia. Most clinicians acknowledge this. Few consistently see it.
Why human observers “miss” the uterus
The uterine tracing is visually blunt. The toco is notoriously inaccurate in high BMI. Resting tone is often guessed rather than measured. Contraction frequency is eyeballed. Duration is rarely timed. Stacking is easily overlooked. Abnormal morphologies—double-peaked, plateaued, prolonged—blend into the background. Tachysystole often becomes visible only after it is severe. And because charting, alarms, and lawsuits all revolve around the fetal heart rate, clinicians naturally invest their attention there.
The result is a paradox. We interpret fetal patterns without fully understanding the contractions driving them.
Generative AI can change this. It does not skim. It measures. It quantifies what humans approximate. It detects what humans overlook. And it integrates both signals continuously.
What generative AI can do for fetal monitoring
1. See the uterus with precision that humans cannot achieve reliably
AI can measure contraction frequency to the second.
It can quantify relaxation intervals.
It can identify rising resting tone.
It can detect prolonged or atypical contraction shapes.
It can notice early tachysystole long before the clinician registers it.
It can correlate each uterine change with the evolving fetal response.
This restores physiologic logic to monitoring. It tells clinicians not just what the fetal heart rate is doing, but why.
2. Interpret CTG holistically, not in fragments
AI can analyze both signals simultaneously. It can recognize when “late decelerations” are not late at all, but rather the predictable output of excessive uterine workload. It can distinguish between genuine fetal acidemia and reversible uterine stress patterns. It can identify patterns caused by oxytocin titration, maternal hypotension, hyperstimulation, or poor uterine relaxation.
Obstetricians have always tried to do this. AI simply does it earlier, faster, and more accurately.
3. Reduce false alarms and enhance situational awareness
Instead of relentless alarms and manual scrolling through hours of strips, AI can summarize:
• How the baseline has changed
• Whether variability is trending downward
• What contraction frequency and intensity have done
• Whether decelerations are worsening or evolving
• What events correspond to oxytocin adjustments
• Whether the fetus is adapting or losing reserve
Clinicians remain in control. But the noise drops and the picture sharpens.
4. Support high-stakes decisions during deteriorating patterns
When the tracing worsens and the room fills, AI can deliver a two-sentence explanation of the physiologic trajectory: whether uterine stress is the primary driver, whether fetal recovery is lengthening, and whether the pattern is reversible. It can provide the clarity that clinicians often struggle to articulate under pressure.
How an ObGyn can use GAI today, with nothing but an iPhone
You do not need an enterprise platform to use AI meaningfully. A clinician can take a clear iPhone photo of the strip, crop out identifiers, and upload it to a secure generative-AI tool. The prompt should be explicit: “Describe the baseline, variability, accelerations, decelerations, contraction frequency, contraction duration, resting tone, and relaxation interval. Identify any abnormal uterine patterns. Explain how the fetal response relates to the contraction pattern. Suggest reasonable next steps for conservative management.”
The AI will not issue a medical order. It will produce a structured physiologic interpretation including the uterine contribution, which is exactly what clinicians miss most often when fatigued. The physician then verifies the analysis and uses it to refine judgment. This is not replacing expertise. It is augmenting it with consistency and vigilance.
A useful analogy
AI is not a robotic second opinion. It is the resident who never looks away from the strip, never gets tired, never loses count of contractions, and never forgets the last two hours. It hands you the physiologic synthesis you would produce yourself if you had unlimited attention.
What is new and easily overlooked
The breakthrough is not classification accuracy. It is narrative physiology.
AI can explain:
• “Variability narrowed steadily during increasing contraction frequency.”
• “Resting tone rose 10 mmHg over the last hour.”
• “Recoveries are lengthening.”
• “The tracing improved briefly after repositioning but worsened with ongoing tachysystole.”
For the first time, AI can make the uterine driver visible again.
Reflection
Obstetrics is defined by timing. The right adjustment at the right moment prevents harm. Generative AI provides steady eyes on both signals, restoring the dual nature of intrapartum physiology. It does not remove the clinician. It restores the clinician’s situational awareness. The ethical question ahead is simple: will we allow technology to help us see what we have always intended to see but often cannot? If the answer is yes, labor and delivery will be safer for mothers and babies.