When Risk is Tiny, But Policy is Loud: The Inconsistencies of Acetaminophen and Home Birth
Home births are far riskier both in absolute and relative term than untreated fever in pregnancy
Medical ethics demands consistency. If we ask patients to make informed decisions, then the way we frame risk must be coherent, transparent, and based on numbers as well as values. Yet professional societies often fall into a pattern of exaggerating small risks while minimizing large ones, depending on the political or cultural context. Two examples illustrate the problem: acetaminophen use in pregnancy, and home birth.
Fever, Acetaminophen, and Neural Tube Defects
The American Academy of Pediatrics (AAP) has argued that pregnant patients should use acetaminophen to control fever, because untreated fever in early pregnancy is associated with an increased risk of neural tube defects (NTDs). The logic is clear: fever is potentially teratogenic, so lowering temperature reduces that risk.
But let us look closely at the numbers. Meta-analyses show that maternal fever in the critical 4th gestational week is associated with about a twofold increased risk of NTDs【Dreier 2014; Feldkamp 2010】. Since the baseline risk of NTDs in the United States is roughly 0.05–0.1% (5–10 per 10,000), doubling it still results in only 0.1–0.2% (1–2 per 1,000 pregnancies). The absolute increase is very small. Moreover, this vulnerable period lasts only about one week—days 21–28 after fertilization—when the neural tube closes.
In other words, the AAP’s position makes sense biologically, but the absolute risk is tiny. Yet acetaminophen is promoted as a necessary intervention because of that tiny increase.
Home Birth and Neonatal Mortality
Now compare this with how the same organization discusses home birth. Data from multiple large studies show that planned home births carry a neonatal mortality risk that is nearly tenfold higher than hospital births (Our study). Instead of 0.05% neonatal mortality, the number rises closer to 0.5%. That is an absolute difference of 0.45 percentage points—nine times larger than the fever/NTD difference.
And yet the AAP, while acknowledging the risk, describes home birth as an acceptable option, even characterizing the absolute increase in mortality as “small.” The inconsistency is striking: a 0.1% NTD risk is treated as intolerable, but a 0.5% neonatal death risk is minimized.
The Ethical Problem
This reveals a troubling asymmetry. When a recommendation aligns with cultural comfort—such as promoting a common, over-the-counter medication—professional societies emphasize even tiny absolute risks to justify intervention. When a recommendation conflicts with cultural or political sensitivities—such as criticizing home birth more forcefully—those same societies downplay much larger risks.
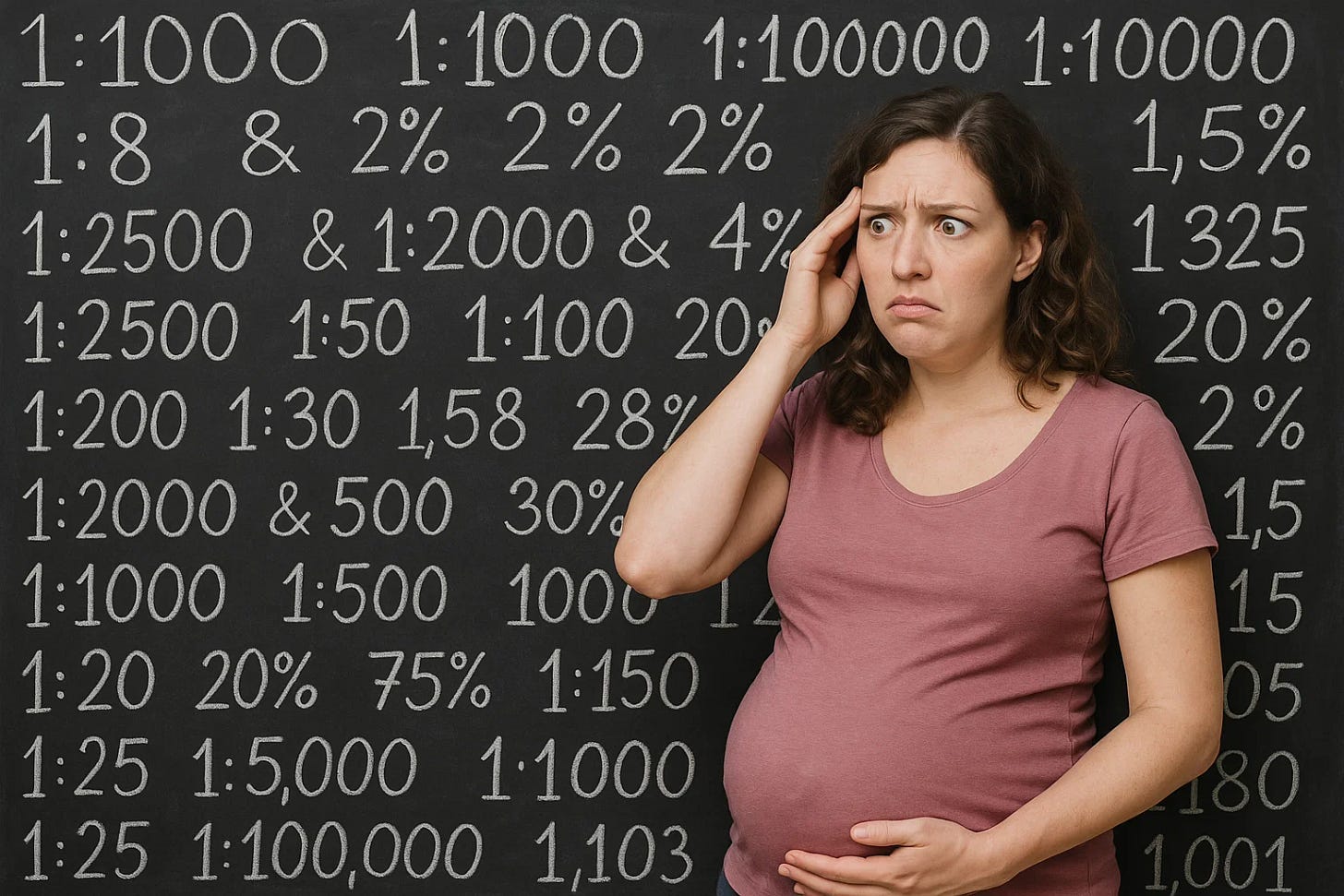
For patients, this creates confusion and undermines trust. If risk communication is inconsistent, how can patients believe that they are truly being told the whole truth? And for physicians, the inconsistency undermines our ethical obligation to practice based on evidence, not convenience or politics.
What We Owe Our Patients
Ethically, we owe patients transparency about both relative and absolute risk. Fever does double the relative risk of NTDs, but the absolute increase is very small. Home birth increases neonatal mortality tenfold, and the absolute increase is far larger. Patients can handle this truth if it is explained clearly. What they cannot handle is being told that a small risk is urgent while a much larger one is negligible.
Our responsibility is to present risks consistently, to respect autonomy, and to avoid letting external pressures shape how we describe evidence. Whether the topic is acetaminophen, home birth, or any other intervention, the numbers must be placed in their full context.
Closing Reflection
Medicine must be honest not only about science, but also about the way we frame science. If professional organizations want to preserve trust, they need to align their messaging: treat small risks as small, and large risks as large. Anything else undermines both patient autonomy and professional credibility