When Morbidity Speaks: What a New Mortality-Weighted Index Reveals About How Women Survive Childbirth
A new study shows that nearly every maternal death is preceded by measurable warning signs. The question is whether our systems are prepared to listen.
A new paper in BMC Pregnancy and Childbirth has quietly delivered one of the most important conceptual shifts in maternal health measurement in more than a decade.
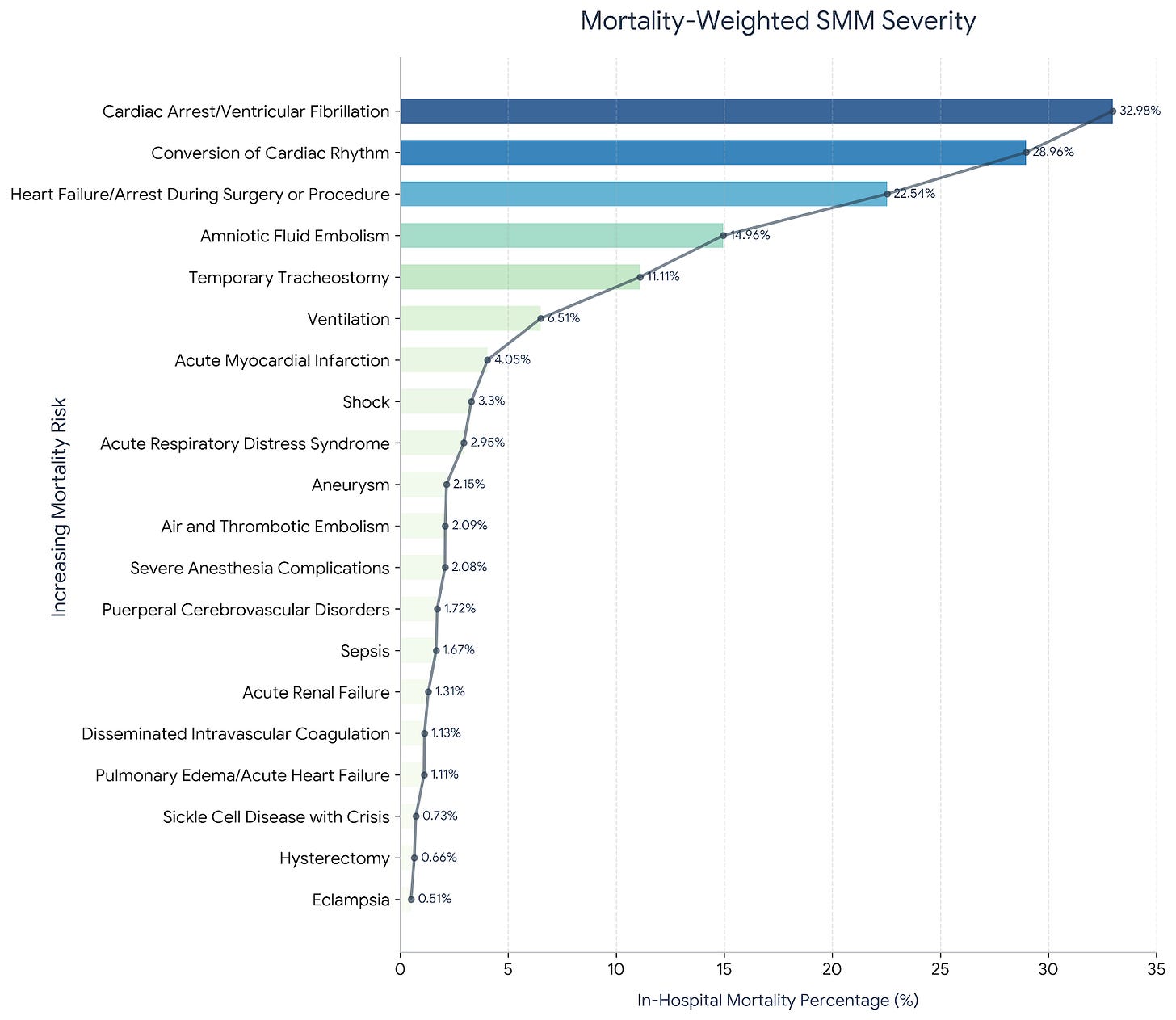
The study, Mortality-Weighted Severe Maternal Morbidity: A Novel Approach to Assessing Maternal Health Outcomes, was received on August 12, 2025 and accepted on November 21, 2025. It proposes a simple yet transformative idea. Not all complications in childbirth are equal. Some confer a risk of death thirty times greater than others. Yet our national severe maternal morbidity (SMM) measure treats all indicators as a binary yes or no. The result is a tool that hides the very information clinicians need most: the true gradient of danger.
The authors analyzed more than 7.1 million inpatient deliveries. Ninety-six percent of women who died had at least one SMM indicator beforehand. Some indicators carried mortality rates of thirty percent. Others carried less than one percent. By weighting each indicator according to its conditional probability of in-hospital death, the researchers created a continuous risk score that provides nuance our current system lacks. For clinicians who have lived these events, the results feel both validating and sobering.
This essay explains what the new index means, why it matters, and how the twenty SMM indicators function as a roadmap of clinical deterioration that we can no longer afford to ignore.
Understanding the New Mortality-Weighted Index
The classic CDC SMM index is binary. Either a complication is present or it is not. This approach offers simplicity but sacrifices clinical truth. It treats cardiac arrest and eclampsia as equal contributors to morbidity. It tells us nothing about severity, clustering, or additive risk.
The new mortality-weighted SMM index (w-SMM) restores the missing dimension. It assigns weights to each indicator based on its observed probability of maternal death. Scores range from 0 to 1, with higher values reflecting greater mortality risk. Women with multiple indicators accumulate risk quickly. In the study, those with five or more SMM indicators had a sixteen percent mortality rate. That is not a rare catastrophe. It is a predictable clinical trajectory.
What makes the w-SMM compelling is its alignment with real bedside experience. Clinicians know that ventilation plus DIC plus shock behaves differently than any one event alone. They know that cardiac arrest is not the same as sepsis. Now the data reflect that lived reality.
The Twenty SMM Indicators: What They Signal and Why They Matter
Below is a clear summary of the twenty SMM indicators that shape the new index. Each represents a moment of profound vulnerability.
1. Cardiac Arrest or Ventricular Fibrillation.
The highest-risk event. Survival depends on immediate CPR, uterine displacement, and rapid delivery if needed. Prevention lies entirely in recognizing decompensation before arrest occurs.
2. Conversion of Cardiac Rhythm.
Required cardioversion signals life-threatening electrical instability. Pregnancy amplifies arrhythmia risk. Early ECG workup of palpitations or syncope prevents escalation.
3. Heart Failure or Arrest During Surgery.
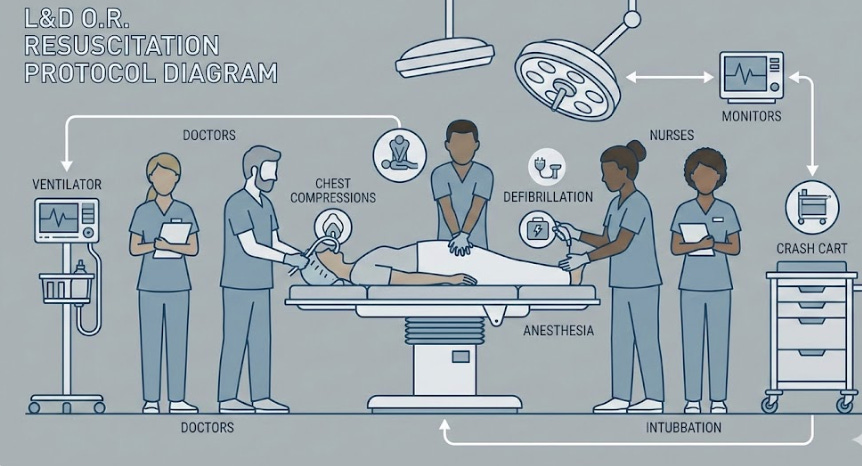
Often related to hemorrhage, cardiomyopathy, or anesthetic complications. Prevention demands skilled anesthesia, preoperative risk evaluation, and rapid-response rehearsal.
4. Amniotic Fluid Embolism.
Rare, abrupt, and often fatal. There is no prevention, only preparedness. Massive transfusion and coordinated support must be available immediately.
5. Temporary Tracheostomy.
Marks severe, prolonged respiratory failure. Prevention requires early airway assessment, thoughtful ventilatory management, and timely escalation.
6. Ventilation.
Mechanical ventilation reflects significant respiratory compromise from infection, hemorrhage, or preeclampsia. Early recognition of oxygenation decline is critical.
7. Acute Myocardial Infarction.
Pregnancy-associated MI often stems from coronary dissection or thrombosis. Chest pain in pregnancy must never be minimized.
8. Shock.
The final common pathway of inadequate tissue perfusion. Early lactate measurement and rapid activation of hemorrhage or sepsis pathways save lives.
9. Acute Respiratory Distress Syndrome.
Often related to sepsis, aspiration, or transfusion. Prevention centers on infection control, careful transfusion, and early respiratory support.
10. Aneurysm.
Pregnancy can precipitate rupture in undiagnosed aortopathy. Screening high-risk women and strict blood pressure control reduce risk.
11. Air and Thrombotic Embolism.
Reflects vascular access errors or hypercoagulability. Prevention requires meticulous technique and consistent VTE prophylaxis.
12. Severe Anesthesia Complications.
Includes airway collapse and high spinal block. Prevention lies in experienced teams, airway assessment, and simulation training.
13. Puerperal Cerebrovascular Disorders.
Stroke risk increases with hypertension and preeclampsia. Neurologic symptoms must always be treated as emergencies.
14. Sepsis.
Maternal sepsis can evolve quickly and silently. Prevention requires attention to early signs and immediate antibiotics.
15. Acute Renal Failure.
Often reflects preeclampsia, hemorrhage, or sepsis. Prevention depends on blood pressure control and adequate perfusion.
16. Disseminated Intravascular Coagulation.
Triggered by hemorrhage, abruption, or AFE. Rapid transfusion guided by labs is essential.
17. Pulmonary Edema or Acute Heart Failure.
Frequently caused by preeclampsia or fluid overload. Prevention is strict fluid management and rapid recognition of dyspnea.
18. Sickle Cell Disease With Crisis.
Crisis poses high risk of hypoxia and infection. Prevention includes hydration, early pain management, and infection control.
19. Hysterectomy.
Usually reflects life-threatening hemorrhage or placenta accreta spectrum. Prevention depends on antenatal diagnosis and planned delivery in expert centers.
20. Eclampsia.
Represents unchecked preeclampsia. Prevention is timely blood pressure screening and magnesium sulfate when indicated.
Why the Weighted Index Matters Now
The mortality-weighted SMM index does more than improve surveillance. It exposes the hierarchy of danger that clinicians understand intuitively but that national metrics have flattened. It tells hospitals where patients fall on a risk continuum rather than offering a simple yes or no. It clarifies that nearly every maternal death is preceded by a measurable signal. The remaining challenge is whether we invest in systems capable of detecting those signals early.
For a field struggling with rising morbidity and persistent racial inequities, this index is not just a technical achievement. It is a call for better clinical anticipation, more transparent reporting, and more honest understanding of when women are truly at risk.
Reflection
The study’s most unsettling finding may also be its most hopeful. Almost all maternal deaths were preceded by identifiable conditions. That means maternal mortality is rarely sudden and never unknowable. The question is no longer whether warning signs existed. It is whether we are prepared to act when they appear.


What strikes me is how the w-SMM essentially codifies what frontline clinicians already know intuitively but the data systems kept erasing. The finding that 96% of maternal deaths had prior SMM indicators is both reassuring and frustrating, it shows the warning signs are there but we're not built to respond early enough. I've seen similar issues in other high-stakes settings where binary metrics flatten risk gradients and make it harder to prioritize interventions. The clustering insight is probably the most actionable bit, knowing that multiple indicators accelerate risk geometrically changes triage completely.