She cancels plans the week before her period. Not because she doesn’t want to see her friends, but because she knows she’ll say something she regrets. The irritability feels like a switch flipping. The sadness comes from nowhere. Her partner has learned to give her space, but she hates that he has to.
Her doctor told her it was “just PMS.” Take some ibuprofen. Maybe try yoga.
This is the problem. Premenstrual disorders are real, treatable conditions. Yet many women suffer for years without knowing that effective treatments exist.
What Are Premenstrual Disorders?
Premenstrual disorders include a spectrum of symptoms that follow a predictable pattern: they appear during the luteal phase (the two weeks between ovulation and menstruation), then resolve within a few days of bleeding. This cyclical timing is what separates premenstrual disorders from other conditions like depression or anxiety, which persist throughout the month.
The symptoms fall into two categories.
Mood symptoms include irritability, anger, mood swings, sudden sadness or tearfulness, sensitivity to rejection, depressed mood, and anxiety or tension.
Physical symptoms include difficulty concentrating, fatigue, changes in appetite or food cravings, sleep problems, breast tenderness, joint or muscle pain, and bloating.
The underlying biology involves hormonal fluctuations during the menstrual cycle. Estrogen levels rise and fall in the luteal phase, which can disrupt serotonin regulation in the brain. Some women also have heightened sensitivity to allopregnanolone, a metabolite of progesterone. These hormonal shifts don’t cause problems for everyone, but for susceptible women, they trigger significant symptoms.
PMS (premenstrual syndrome) is diagnosed when any combination of these mood or physical symptoms occurs in a cyclical pattern and interferes with daily life. PMDD (premenstrual dysphoric disorder) is more severe and has specific diagnostic criteria from the DSM-5: at least 5 symptoms must be present in the week before menstruation, including at least 1 mood symptom and 1 physical symptom. These symptoms must substantially decrease or resolve within a week after menstruation begins.
Diagnosis requires tracking symptoms daily for at least two consecutive menstrual cycles using a validated tool like the Daily Record of Severity of Problems. This documentation confirms the pattern and rules out other conditions. Many women suspect they have PMDD but haven’t tracked their symptoms systematically. The tracking itself can be revealing: some women discover their symptoms don’t actually follow the luteal pattern, which points toward a different diagnosis. Others finally have proof that what they’ve experienced for years is real and has a name.The Numbers
PMS affects about 1 in 4 menstruating women. That’s common enough to be dismissed as “normal.”
PMDD (premenstrual dysphoric disorder) is different. It affects 2-5% of women and causes severe mood symptoms: irritability that destroys relationships, depression that makes work impossible, anxiety that feels unbearable. These symptoms appear in the week before menstruation and disappear within days of bleeding. The pattern is the diagnosis.
A new JAMA synopsis of ACOG guidelines, published this week, confirms what the evidence shows: we have treatments that work. The question is whether women know about them.
What Actually Works
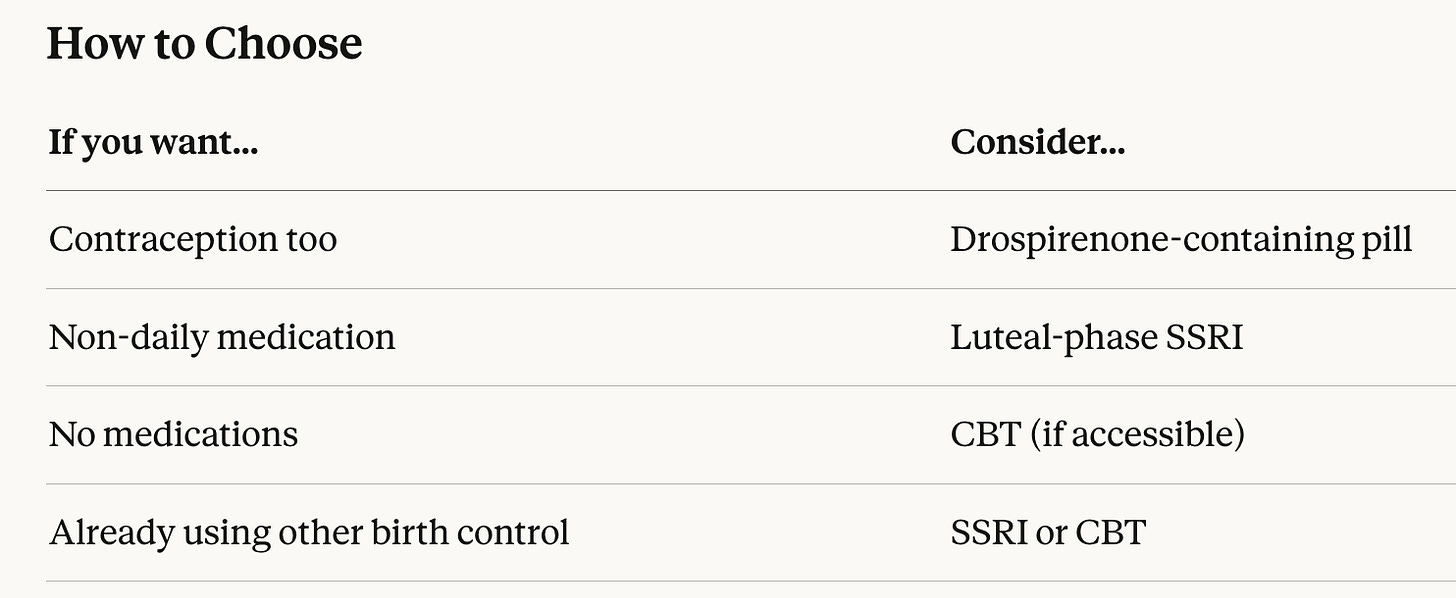
SSRIs (antidepressants) are first-line treatment for mood symptoms. Here’s what most women don’t know: you don’t have to take them every day. Luteal-phase dosing means starting the medication at ovulation and stopping when your period begins. This works for many women and avoids the side effects of daily use.
The data: escitalopram 20mg reduced irritability by 80% compared to 30% with placebo. A 2024 Cochrane review of 12 trials found both continuous and intermittent dosing effective, with continuous slightly better.
Birth control pills containing drospirenone (brand names include Yaz and Beyaz) are the only oral contraceptives FDA-approved for PMDD. In trials, 48% of women responded to treatment versus 36% on placebo. The number needed to treat is 8, meaning for every 8 women who try it, one will benefit who wouldn’t have improved on placebo.
Cognitive behavioral therapy works too. An 8-week internet-based CBT program cut the percentage of women meeting PMDD criteria from 81% to 41%. Benefits lasted at least 3 months after treatment ended.
Most women benefit from combining approaches: lifestyle changes (exercise, sleep, stress management) plus medication or therapy.
The Real Problem
The evidence is clear. The treatments are available. So why do women suffer?
Because we’ve normalized premenstrual misery. Because “it’s just hormones” has become a way to dismiss women’s symptoms rather than treat them. Because many clinicians don’t ask, and many women don’t know they can ask.
If your symptoms interfere with your work, your relationships, or your quality of life, that’s not something you should just push through. Track your symptoms for two cycles. If the pattern fits, bring the data to your doctor.
You deserve more than “just deal with it.”
Reference: Ortiz Worthington R, Eastman LM, Alexander JT. Management of Premenstrual Disorders. JAMA. Published online February 4, 2026. doi:10.1001/jama.2025.26054