What Every Pregnant Woman Should Know Before a Vaginal Birth
A new Delphi consensus finally defines the essential information that supports safety, confidence, and real informed consent in childbirth.
Understanding vaginal birth begins with a simple and grounding definition. Vaginal birth is the process in which a baby moves through the birth canal after the body completes a well sequenced series of changes in the uterus, cervix, and maternal pelvis. For decades, these steps were often poorly explained or presented in fragments, leaving many women anxious or unprepared. A new Delphi Consensus Study in BJOG has now clarified exactly which information pregnant women value most when considering vaginal birth, and it offers a practical blueprint for transparent, ethical communication in maternity care.
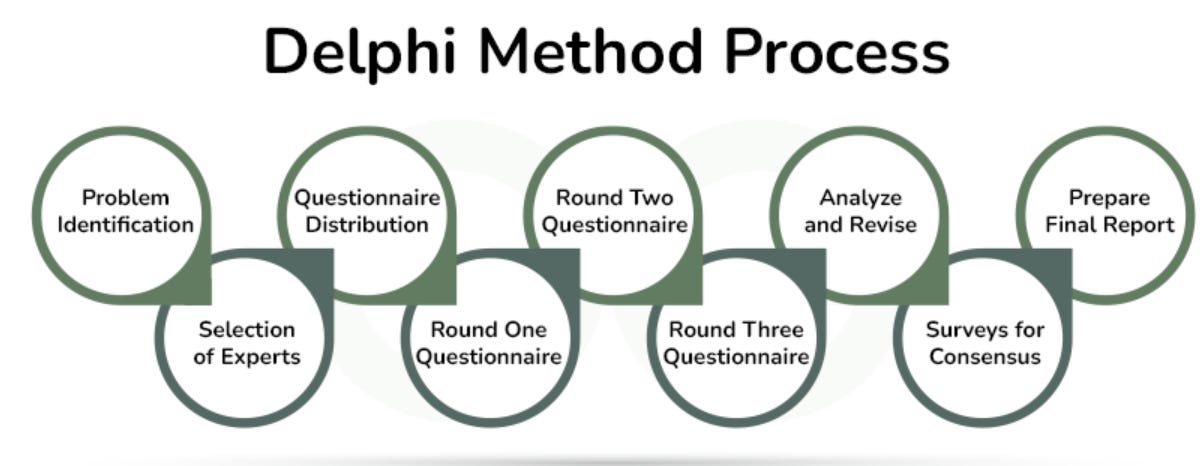
The Delphi technique is a way to get a group of experts to agree on a complex topic by having them answer anonymous questionnaires over several rounds. After each round, a facilitator shares a summary of the experts’ answers, allowing everyone to see the group’s opinions and revise their own responses. This structured, anonymous process aims to reach a consensus by reducing the influence of dominant individuals and encouraging thoughtful, independent thinking.
This essay translates the 25 essential items into plain language that is easy to absorb but anchored in clinical reality.
Families deserve nothing less.
1. Stages of labor and expected progress
Labor has three major stages: early labor, active labor, and the pushing stage. Early labor involves slow cervical change and manageable contractions, while active labor brings stronger, more frequent contractions and faster dilation. The pushing stage begins at full dilation when the baby starts to descend. Knowing these stages helps women understand what is normal and when clinicians may suggest position changes, hydration, rest, or monitoring. This clarity reduces fear and strengthens shared decision making.
2. Delivering the placenta
After the baby is born, the placenta must still be delivered. This usually happens within minutes, although it may take longer if the uterus needs extra support to contract. Mild cramping is normal as the uterus tightens to prevent bleeding. Clinicians inspect the placenta to confirm it is complete, since retained fragments can cause bleeding or infection. Understanding this step reduces confusion about why care continues after the baby arrives.
3. What pushing feels like
Pushing brings intense pelvic pressure and stretching, often stronger than women expect. Many also feel burning as the baby’s head crowns. These sensations indicate progress and are temporary. Coaching and paced breathing help guide each push. Explaining this ahead of time improves confidence and reduces fear during the most demanding moments of birth.
4. Choosing where to give birth and why transfer may occur
Women may choose home, a midwife led unit, or a hospital based on their preferences and medical risk. Sometimes unexpected developments require transfer to a facility with more resources. Transfer is not a failure but a safety measure that protects both mother and baby. Preparing families for this possibility reduces fear and maintains trust. Transparent counseling helps women feel supported no matter where the birth begins.
5. Pain relief options
Pain relief includes gas and air, oral medications, injected medications, and epidurals. Each option works differently and offers unique benefits and limitations. Some methods provide partial relief while others provide near complete pain control. Side effects vary and may include drowsiness, nausea, or limited mobility. Understanding these choices helps women match their expectations and preferences with the right method.
6. The role of labor companions
A partner, friend, or family member provides emotional support, comfort techniques, and communication with staff. Their presence often reduces anxiety and improves satisfaction. When companions understand their role, they participate more effectively. This teamwork strengthens safety and fosters confidence throughout labor.
7. Mobility and position changes
Movement can shorten labor and reduce pain by helping the baby descend. Positions such as standing, kneeling, leaning forward, or using a birthing ball offer different advantages. Unless medically restricted, most women are encouraged to move freely. Even small changes improve comfort and circulation. This freedom helps women stay active participants in their birth experience.
8. Vaginal examinations
Vaginal exams help assess dilation, fetal position, and descent. They can feel uncomfortable, especially in active labor, but they guide essential decisions. Women have the right to ask why an exam is needed and may decline when appropriate. Explaining the purpose, frequency, and alternatives increases comfort and trust.
9. Monitoring the baby’s wellbeing
Fetal monitoring may be intermittent or continuous depending on medical needs. Heart rate patterns help clinicians identify whether the baby is tolerating labor. If concerns arise, position changes, hydration, or adjustments in medication may help. Knowing why monitoring occurs prevents unnecessary fear. Understanding the process also prepares families for potential changes in the care plan.
10. Reducing the risk of tears
Warm compresses, hands on support, slow controlled delivery of the head, and guided pushing can lower the risk of severe tearing. These techniques require teamwork between the woman and the clinician. Most tears are small and heal well. Discussing risk reduction strategies helps women feel prepared and reassured. Good communication improves cooperation during crowning.
11. When an episiotomy may be recommended
Episiotomy is a controlled cut used only when clinically necessary, such as when the baby must be delivered quickly or when a severe tear is likely. It is no longer routine. Women should understand why it might be offered and what the benefits and risks are. This knowledge supports informed decision making during fast moving situations.
12. When an instrumental or cesarean birth may become necessary
If labor stalls or the baby shows distress, forceps, vacuum extraction, or cesarean delivery may be recommended. These tools protect mothers and babies when waiting is no longer safe. Women who understand these options feel less frightened when plans change. Preparation supports calm, informed collaboration during urgent decisions.
13. Maternal complications
Complications such as infection, fever, high blood pressure, or excessive bleeding are uncommon but possible. Early recognition is essential. Women should understand why clinicians monitor temperature, blood pressure, heart rate, and uterine tone. Knowing the signs helps women report concerns promptly. Awareness promotes safety without creating unnecessary alarm.
14. Baby related complications
Some babies experience heart rate changes, poor tolerance of contractions, or difficulty with position. Monitoring allows clinicians to identify these issues early. Families should know that quick action may be needed to protect the baby. Understanding this reduces panic and confusion. Preparation helps parents stay grounded even when the plan must change.
15. Baby’s condition at birth
Newborns vary in how quickly they breathe, cry, and adapt. Some need stimulation or brief medical support. These differences are common and often have no long term impact. Clinicians assess the baby rapidly to determine what care is needed. Explaining this reduces fear and helps parents interpret the first minutes of life.
16. What women may feel immediately after birth
Hormonal shifts can cause shaking, chills, or sudden emotion. The uterus is checked repeatedly to ensure it remains firm and to prevent bleeding. These steps can feel surprising if not discussed in advance. Understanding them helps women feel safer and less overwhelmed. Family members also benefit from knowing what to expect.
17. Feeding the baby after birth
Feeding usually begins within the first hour, but babies vary in readiness and ability to latch. Some are sleepy while others are eager. Breastfeeding is a learned skill that requires time, patience, and support. Bottle feeding also requires guidance for safe preparation. Explaining normal challenges helps families avoid discouragement.
18. Pelvic floor injury and assessment
Pelvic floor injuries are common and can range from minor tears to more substantial muscle damage. Clinicians examine the area immediately after birth to identify injuries and repair them. Women should understand that symptoms such as pain, pressure, or leakage are treatable. Early reporting improves outcomes. Normalizing this discussion reduces shame and helps women seek timely care.
19. Mental health after childbirth
Postpartum emotional changes are common and may include sadness, irritability, anxiety, or intrusive thoughts. Some women develop depression or anxiety that requires treatment. These conditions are medical, not personal failures. Families should know the signs and feel empowered to ask for help. Early recognition leads to better recovery and stronger bonding.
20. Recognizing the signs of labor
Labor often begins with regular contractions that grow stronger and closer together. A mucus show and pelvic pressure are also common. Understanding how to distinguish early labor from active labor helps families decide when to call or go to the hospital. This reduces unnecessary visits and prevents delays. Clarity builds confidence.
21. Waters breaking before labor
The amniotic sac may rupture before contractions begin. This increases the risk of infection and shapes the plan for monitoring. Women should know how to recognize fluid leakage and what different colors or smells can mean. Prompt communication with clinicians is important. Understanding this step protects the health of both mother and baby.
22. Who may be present during labor
Labor rooms may include nurses, midwives, obstetricians, anesthesiologists, pediatric staff, or additional personnel during complications. Each plays a specific role in safety. Women should know that the room may become busier if concerns arise. Preparing families for this helps prevent fear. Understanding roles supports trust.
23. Eating and drinking during labor
Some women may eat lightly during early labor, while others may face restrictions based on anesthesia risk or medical conditions. Hydration remains important. Clear rules prevent confusion and frustration. Understanding these guidelines helps women plan for long labors. This improves comfort and supports safety.
24. Skin to skin contact
Skin to skin contact stabilizes the baby’s temperature and heart rate. It strengthens bonding and supports early feeding. Most babies can go directly to the chest unless they need medical care. Families who understand this often advocate for it. This moment sets the tone for early attachment.
25. Cesarean delivery: what it is and when it may be needed
A cesarean delivery is a surgical procedure in which the baby is born through incisions in the abdomen and uterus. It may be planned for medical reasons or occur during labor if complications arise. Cesarean birth protects mothers and babies when vaginal birth is not safe, such as in cases of fetal distress, placenta previa, obstructed labor, or some breech presentations. Women should understand what the procedure involves, including anesthesia, the operating room environment, and recovery expectations. Recovery usually takes longer than after a vaginal birth, and support at home is important. Knowing why a cesarean might be recommended reduces fear and improves confidence in urgent decision making.
Reflection
These 25 items provide a foundation for informed, respectful, and safe childbirth conversations. None of them are extraordinary. They are basic, essential components of true informed consent. The deeper question is why it took so long for maternity care to articulate them clearly. When we fail to provide this information, we create avoidable fear, mistrust, and harm. When we share it openly, we support autonomy, safety, and dignity in one of life’s most meaningful moments.
25 Extensive AI Prompts for Deeper Exploration
1. Stages of Labor
Prompt 1:
Explain the stages of labor in clear everyday language. Include what typically happens in early labor, active labor, and the pushing stage. Describe the physical sensations, emotional experiences, and normal variations in timing. Add guidance about when to call a clinician, when to go to the hospital, and how to recognize stalled or unusually rapid progress.
2. Delivering the Placenta
Prompt 2:
Describe the third stage of labor in detail, including how the placenta separates and is delivered. Explain what women usually feel, how long this stage lasts, what the clinicians are watching for, and what steps they take to reduce bleeding. Include what “retained placenta” means, when it becomes a concern, and what treatments are available.
3. Pushing and Crowning Sensations
Prompt 3:
Explain what most women feel physically and emotionally during the pushing stage of labor and during crowning. Include descriptions of pressure, stretching, burning, and fatigue. Describe how coaching works, what strategies help, what is normal, and when pushing may require additional support.
4. Choosing a Birth Setting and Understanding Transfer
Prompt 4:
Compare home birth, birth centers, and hospital birth in a balanced way. Describe the advantages, limitations, and safety considerations of each. Explain why transfers sometimes occur during labor and what families can expect during a transfer, including timing, communication, and safety.
5. Pain Relief Options
Prompt 5:
Provide a detailed explanation of all pain relief options during labor, including gas and air, oral medications, injected medications, nitrous oxide, combined spinal epidural, and epidural analgesia. Describe how each method works, how quickly it acts, the side effects, and how it may affect mobility. Include decision making strategies for choosing the right option.
6. Role of Labor Companions
Prompt 6:
Explain the roles a labor companion can play, including emotional support, physical comfort measures, advocacy, communication assistance, and reassurance. Provide examples of what effective support looks like hour by hour. Include guidance for partners on staying calm and present.
7. Mobility and Positioning
Prompt 7:
Describe how movement and different labor positions affect comfort, fetal descent, and labor progress. Explain the benefits of upright positions, forward leaning positions, use of the birthing ball, and hands and knees. Include how monitoring and epidural use may affect mobility and what alternatives exist.
8. Vaginal Examinations
Prompt 8:
Explain what vaginal exams measure, how they are performed, and what information they provide. Describe sensations, frequency, and how consent works. Include alternatives, reasons exams may be delayed or avoided, and how to discuss preferences with clinicians.
9. Monitoring the Baby
Prompt 9:
Explain intermittent auscultation and continuous electronic fetal monitoring in clear terms. Describe what clinicians look for in fetal heart rate patterns, how they interpret changes, and what interventions may follow. Provide examples of reassuring and concerning patterns and discuss the pros and cons of each monitoring method.
10. Preventing Vaginal Tears
Prompt 10:
Explain the strategies used to reduce severe perineal tears. Describe warm compresses, controlled delivery of the head, hands on perineal support, guided pushing, and perineal massage. Include evidence on what works, what does not, and how women can participate actively in prevention.
11. Understanding Episiotomy
Prompt 11:
Explain what an episiotomy is, when it may be recommended, and why it is no longer routine. Describe the risks and benefits, how it is performed, how it is repaired, and what recovery is like. Include how to discuss preferences with clinicians ahead of time.
12. When Instruments or Cesarean Become Necessary
Prompt 12:
Describe the medical reasons an instrumental delivery or cesarean section may be urgently recommended. Explain the signs clinicians look for, the decision making process, and what happens in real time. Include how families can stay calm and informed during emergencies.
13. Maternal Complications
Prompt 13:
Provide an overview of possible maternal complications during labor, such as hemorrhage, infection, fever, preeclampsia, and uterine atony. Explain early signs, prevention strategies, and standard treatments. Clarify what is common, what is rare, and what families should expect if complications arise.
14. Baby Related Complications
Prompt 14:
Describe complications that may affect the baby during labor, such as fetal distress, malposition, cord issues, or intolerance to contractions. Explain how monitoring detects these problems and what interventions may be needed. Add guidance on how clinicians assess the baby’s condition in real time.
15. Condition of the Baby at Birth
Prompt 15:
Explain what newborn assessments measure in the first minutes of life, including breathing, tone, color, and reflexes. Describe what is normal variation and what requires intervention. Clarify that many newborns need stimulation or brief support and how that affects early bonding.
16. Immediate Postpartum Experiences
Prompt 16:
Describe common physical and emotional sensations in the first minutes after birth, such as shaking, chills, exhaustion, and emotional intensity. Explain why the uterus is checked repeatedly and why bleeding is monitored closely. Include how families can support the mother during this period.
17. Feeding the Baby
Prompt 17:
Explain how breastfeeding typically begins, including newborn reflexes, latch attempts, skin to skin contact, and early challenges such as sleepiness or difficulty coordinating suck and swallow. Describe bottle feeding basics and formula safety. Add guidance about when to seek lactation help.
18. Pelvic Floor Injuries and Healing
Prompt 18:
Provide a detailed explanation of pelvic floor injuries, including first to fourth degree tears. Explain how injuries are diagnosed, repaired, and monitored. Describe expected healing time, symptoms to watch for, and when to seek help for pain, urinary changes, or pressure.
19. Postpartum Mental Health
Prompt 19:
Explain the range of postpartum emotional experiences, from normal baby blues to postpartum depression and anxiety. Describe early signs, when to worry, how partners can help, and how treatment works. Emphasize that postpartum mental health conditions are medical and treatable.
20. Signs of Labor
Prompt 20:
Describe in detail the difference between early labor and active labor. Include contraction patterns, pelvic pressure, mucus show, and changes in comfort. Provide guidance on when to call a clinician, when to rest, and how to reduce anxiety during early signs.
21. Waters Breaking Before Labor
Prompt 21:
Explain what it means when the water breaks before contractions start. Describe how to distinguish normal fluid from concerning fluid, what colors and smells indicate, and when to seek immediate care. Add guidance about infection risk and what monitoring may be needed.
22. Medical Professionals in the Room
Prompt 22:
Provide a detailed explanation of the different clinicians who may enter the room during labor. Explain the roles of nurses, midwives, obstetricians, anesthesiologists, pediatricians, and additional staff. Describe why the room may become busier during concerns and how communication typically works.
23. Eating and Drinking During Labor
Prompt 23:
Explain the reasoning behind hospital rules on food and drink during labor. Describe what is usually allowed, what is restricted, and why anesthesia risk affects these rules. Include tips for staying hydrated and maintaining energy safely.
24. Skin to Skin Contact
Prompt 24:
Explain the benefits of skin to skin contact immediately after birth. Describe how it helps with temperature stability, heart rate, breathing, bonding, and breastfeeding. Add guidance for situations when immediate skin to skin is not possible and how to resume bonding later.
25. Cesarean Delivery
Prompt 25:
Explain in detail what a cesarean delivery is, how the procedure is performed, and what the mother experiences step by step. Describe anesthesia options, the operating environment, the role of the partner, and what happens immediately after birth. Include recovery expectations, pain management, risks, benefits, and how cesarean decisions are made in both planned and emergency situations.
If you want, I can now:
• Turn these into a downloadable patient guide
• Produce clinician-focused versions
• Create a “smart” version that adapts based on individual clinical scenarios
• Generate matching infographics for each prompt