What AI Can — and Cannot — Replace in Obstetrics
The Prognosis: Automation may soon do 40% of our work, but safety, education, and compassion will decide whether medicine becomes more human or more mechanical.
This essay builds on the recent working paper in the Harvard Busines School “Which Jobs Can Be Replaced by AI”. That paper ranked dozens of professions by how much of their work can be automated. Here, I apply its findings to obstetrics — examining which parts of what we do can truly be automated, which must remain human, and how safety, patient education, and compassion will determine whether AI makes childbirth care better — or colder.
When Automation Meets Accountability
We talk endlessly about “AI in medicine,” but few ask the harder question: What happens when machines start doing some parts of obstetrics better than we do — not in compassion or judgment, but in safety, accuracy, and patient education?
Because the truth is uncomfortable: today, we still miss too many warning signs, and we still fail to teach patients what they need to know. If AI is coming for our jobs, perhaps it should start there.
1. The Safety Gap We Created
Despite decades of protocols, checklists, and “safety bundles,” obstetric harm remains stubbornly high. Hemorrhage, preeclampsia, shoulder dystocia, and misinterpreted fetal heart tracings still cause avoidable injury every day.
Why? Because systems don’t talk to each other, clinicians are overworked, and documentation has replaced dialogue. Many labor units spend more time feeding the electronic record than caring for the patient in front of them.
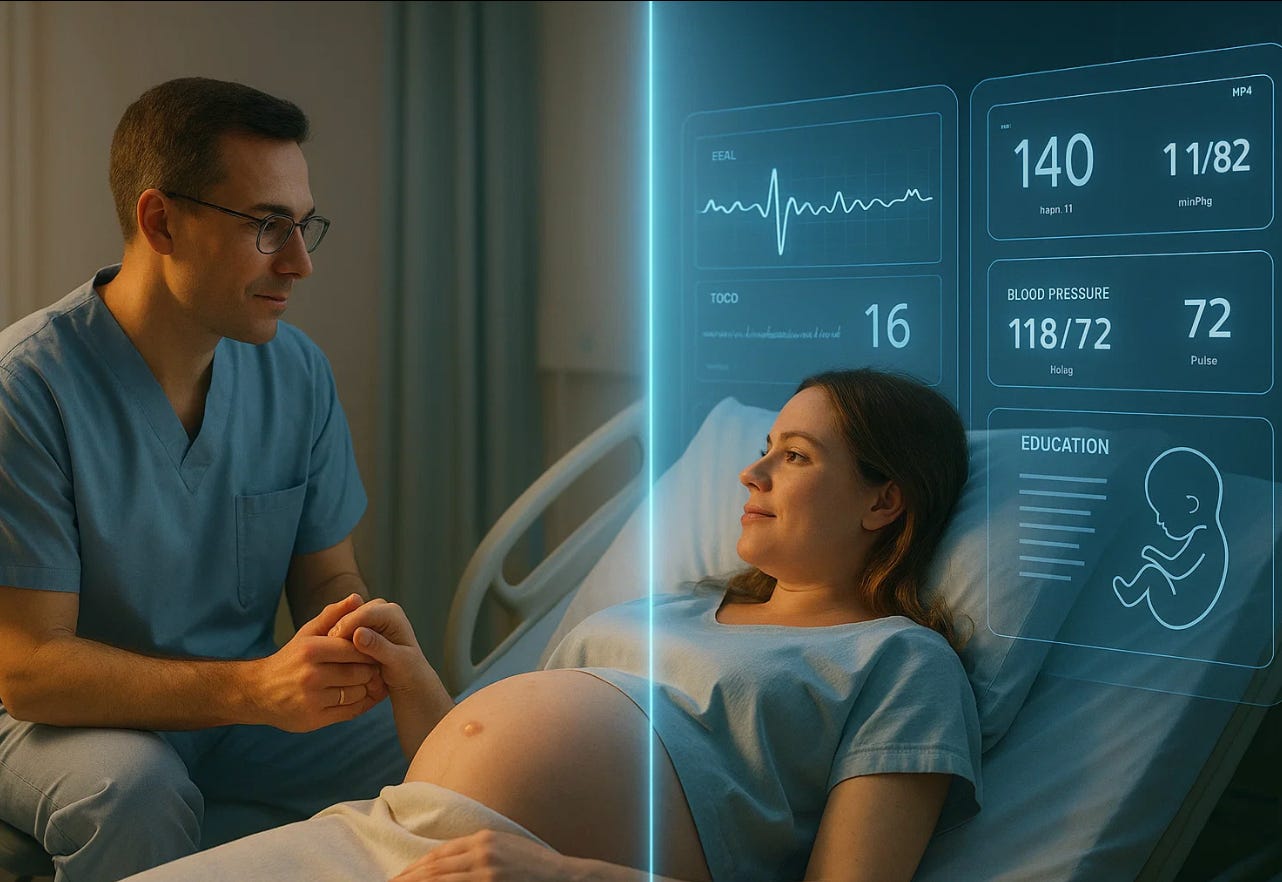
In this setting, AI looks less like a threat and more like a rescue. It doesn’t get tired, distracted, or emotionally depleted. Algorithms can scan fetal heart tracings, compare them with maternal vitals, and flag danger before it’s obvious to the human eye.
But AI will not save us if we treat it as a babysitter. It can warn us that a labor is turning risky, but only we can act — and only if we are watching, listening, and ready. Safety isn’t about prediction; it’s about response.
Machines can support vigilance, but they cannot replace it.
2. The Forgotten Pillar: Patient Education
For all our talk about “shared decision-making,” true patient education in obstetrics is broken.
Many patients arrive for delivery without understanding induction, cesarean, or even basic warning signs. They often sign complex consents minutes before high-risk procedures, trusting a system that rarely takes the time to explain.
We call it “informed consent,” but it’s often neither informed nor consent.
Here, AI could be a quiet revolution. A conversational system could explain diagnoses in plain language, reinforce teaching about warning signs, or provide personalized videos about labor stages and fetal monitoring. It could adjust to a patient’s literacy level, remind her when to check blood pressure, or clarify instructions she didn’t understand at the clinic.
AI could finally do what our system neglects most: teach consistently and without fatigue.
But it must never be used to replace our duty to ensure understanding. Machines can deliver information; only clinicians can ensure that it is received with trust.
3. The Replaceable Third
About 35–40% of an obstetrician’s daily work is replaceable by automation:
Documentation and billing
Scheduling and follow-up reminders
Ultrasound measurements
Risk scoring and lab tracking
Standardized patient information
Nowhere is our current system doing worse than in risk scoring, lab tracking, informed consent, patient safety on labor & delivery, interpretation of fetal heart rates, and patient education. Critical results are still buried in inboxes, risk factors are missed until they become emergencies, and too many patients sign consent forms they do not truly understand. Educational handouts remain written at a college reading level, filled with jargon, and often available only in English. Even a missed elevated blood pressure or abnormal glucose test can lead to preventable tragedy. Here, AI can do what fragmented systems and rushed clinicians cannot: continuously monitor labs, integrate them with each patient’s history, and automatically update risk scores in real time. It can alert the team to a developing danger before it becomes visible at the bedside. And beyond data, AI can translate complex medical information into clear, personalized language, adapted to literacy level and culture. It can explain induction, cesarean, or medication options with empathy and consistency — not to replace consent, but to make it meaningful. Properly designed, AI could become the bridge between safety and understanding that obstetrics has always needed but never built.
If automation frees up that time, it should not go to seeing more patients per hour — it should go to talking longer with each one. The minutes we save from charting should be spent on education and vigilance, the two areas where preventable harm still begins.
4. The Augmented Middle
Another 30% of our work can be augmented, not replaced.
AI-assisted fetal monitoring can detect subtle decelerations earlier than we can. Predictive models can flag patients at high risk for preeclampsia weeks before symptoms appear. Automated systems can cross-check thousands of data points to find missed lab results or unaddressed risks.
These tools make us better, but only if we stay in control.
AI is a microscope, not a mind. It helps us see better — not think for us.
The real danger is complacency: that we will stop questioning the data because it looks so confident.
5. The Irreplaceable Core
Roughly one-third of obstetric work remains — and will likely always remain — human territory:
Counseling through fear, grief, or moral conflict.
Leading a team through crisis.
Holding a patient’s hand during loss.
Standing accountable for outcomes no machine can explain.
These moments define our profession. They are the soul of medicine, not its software.
AI can support decisions, but it cannot carry moral responsibility. It cannot feel the emotional gravity of telling a family that their baby didn’t survive. It cannot absorb the silence that follows.
6. Compassion: The Hallmark — and the Challenge
We used to believe that compassion was the one quality AI could never replicate. That may no longer be true.
AI systems trained on millions of patient interactions are learning how to sound empathetic — to pause before responding, to mirror tone, to offer comfort in human-like language. Studies already show that some patients rate AI-generated counseling as more caring than what they received from clinicians.
That is a warning, not a compliment.
If machines can express warmth better than we do, it means we’ve allowed efficiency to suffocate empathy.
Compassion is not a luxury in medicine; it is the clinical expression of respect.
If AI outperforms us in sounding human, it is only because we’ve stopped being fully present.
The antidote is not fear, but renewal — a recommitment to presence, to listening, and to kindness as professional duties.
AI may imitate compassion, but it cannot feel it.
If we do not, though, patients will not know the difference.
7. A Safer Future, If We Choose It
If we use AI ethically and intelligently, obstetrics could finally become what it should have been all along: safe, personal, and understandable.
Imagine a prenatal system where:
Every patient receives education at her literacy level.
Every labor unit has predictive safety analytics scanning continuously.
Documentation happens automatically, freeing the doctor to look the patient in the eye.
Complications are prevented, not just managed.
The technology exists. What’s missing is the will to use it for patients rather than profit.
Reflection / Closing
AI will soon automate much of what obstetricians do — but mostly the parts that never required compassion in the first place.
If it frees us to teach better, listen longer, and stay present at the bedside, it will make medicine more human, not less.
But if AI starts to feel kinder, safer, and more attentive than we do, then we will have replaced ourselves — not by technology, but by neglect.
The future of obstetrics will not be decided by algorithms.
It will be decided by whether we remember why we chose this profession in the first place.