:We Don’t Live There” Is Not a Scientific Argument. It's Antiscience
How geographic chauvinism quietly undermines evidence-based medicine
The statement is short. It is blunt. And it is astonishingly unserious. Antiscience. Nearly, well like our present government.
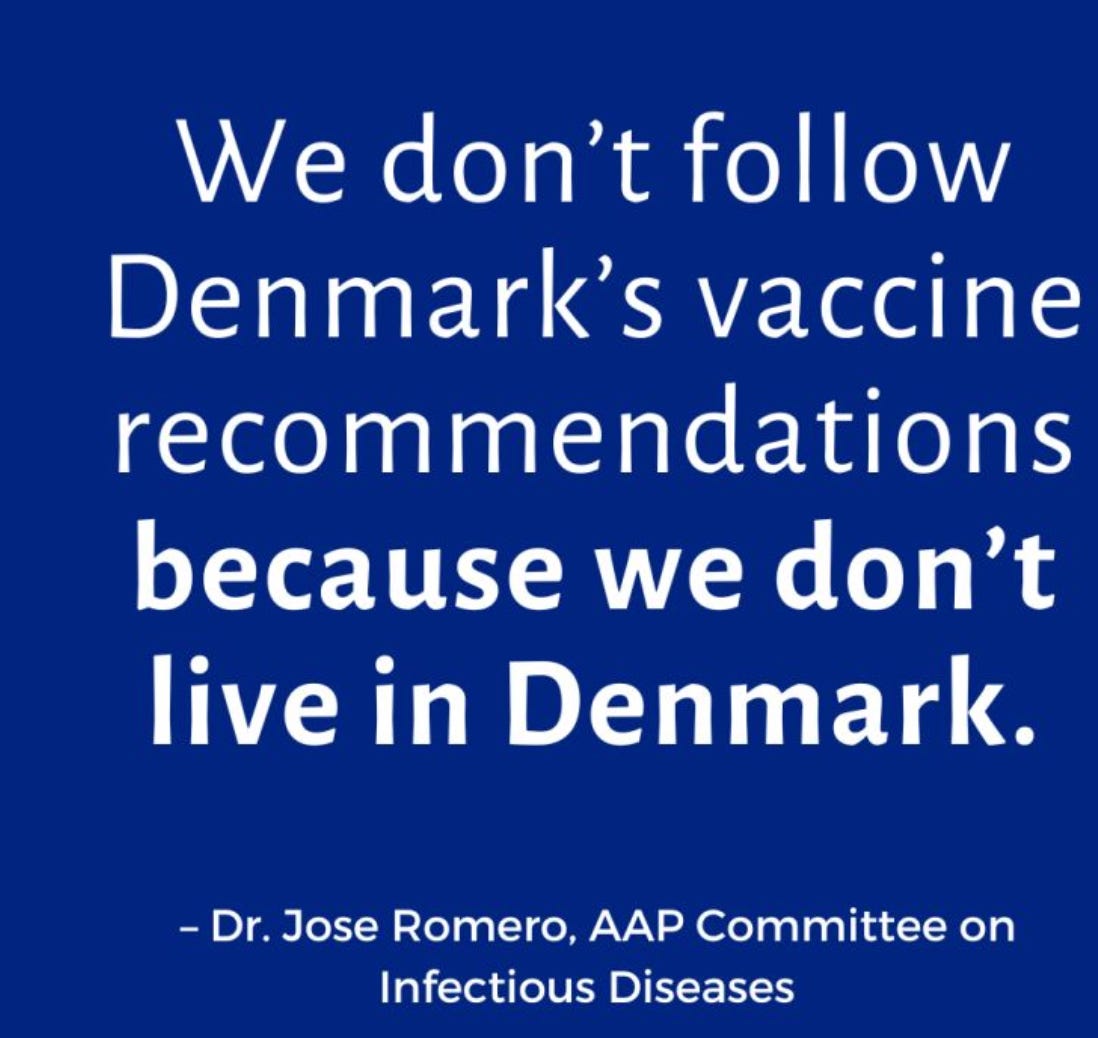
“We don’t follow Denmark’s vaccine recommendations because we don’t live in Denmark.”
This was not a social media troll or a fringe commentator. It was attributed to leadership within the American Academy of Pediatrics (AAP), an organization that claims evidence-based medicine as its moral and intellectual foundation. The problem is not disagreement with Denmark. The problem is the reasoning. Or more precisely, the absence of it.
Let us be clear at the outset. Evidence does not have a passport. Data are not less valid because they cross an ocean. Science does not stop working at customs.
Ooops. Denmark consistently ranks among the top five most livable countries globally due to strong social safety nets, low income inequality, universal health care, and high trust in public institutions, while the United States typically ranks much lower because of greater inequality, fragmented health care, and weaker social protections. That alone should at least prompt humility. Instead, the statement dismisses Danish recommendations not on scientific grounds, but on geography. That is not skepticism. That is parochialism.
This statement confuses geography with evidence. By this logic, we should not follow any international research. No Cochrane reviews from the United Kingdom. No WHO guidelines. No Nordic registry data that forms the backbone of modern perinatal epidemiology. No Canadian outcomes research. No Dutch obstetric trials. No Scandinavian pharmacoepidemiology. The entire global enterprise of medicine collapses under this reasoning.
And yet, we rely on these data constantly. Quietly. Selectively. Often enthusiastically.
Denmark’s universal health care registries often provide data quality that American fragmented systems simply cannot match. That is not an insult. It is an empirical observation.
Denmark can link births, vaccinations, hospitalizations, prescriptions, and long-term outcomes across an entire population with minimal loss to follow-up. The United States cannot. Our data are siloed, payer-dependent, incomplete, and often unavailable for real-time surveillance. Pretending otherwise is self-deception.
When Denmark paused certain vaccines based on pharmacovigilance signals, that was not cultural preference. It was signal detection. Pharmacovigilance exists precisely because rare adverse events do not announce themselves politely. They require large, integrated datasets, rapid analysis, and the institutional courage to pause and reassess when signals emerge.
No single nation has sufficient power to detect rare adverse events quickly on its own. That is why international surveillance exists. That is why post-marketing safety depends on shared data. That is why vaccine safety is a global enterprise. To dismiss another country’s safety signal because “we don’t live there” is to fundamentally misunderstand how modern drug safety works.
This is where the ethical failure of the AAP becomes visible.
Saying “we don’t live there” is an appeal to American exceptionalism, not science. It substitutes national identity for methodological critique. It avoids the hard work of asking the only question that matters. Is the evidence valid?
Instead, it asks a question that is irrelevant. What flag flies over the institution?
This mode of reasoning has consequences. It is the same logic that keeps us clinging to practices abandoned elsewhere, often with outcomes that lag behind peer nations.
Higher maternal mortality. Worse neonatal outcomes in vulnerable populations. Greater disparities. Less trust. More litigation. These are not coincidences. They are the predictable results of systems that resist external learning while insisting on internal superiority.
Evidence-based medicine is not patriotic. It is comparative. It asks what works, where, for whom, and under what conditions. It does not pretend that national borders confer epistemic privilege.
There is also a deeper irony here. The United States routinely urges other countries to follow American guidelines, American regulatory standards, and American clinical frameworks. We export our norms aggressively. But when confronted with high-quality data generated elsewhere, we retreat into insularity. That is not leadership. That is insecurity.
No one is arguing that Denmark’s recommendations must be adopted wholesale without context. Context matters. Baseline risk matters. Health system structure matters. Population characteristics matter. But none of that was addressed in the statement. There was no discussion of study design, signal strength, confidence intervals, or biological plausibility. There was only geography.
That should alarm anyone who cares about scientific integrity.
Professional societies exist to elevate discourse, not to flatten it. They are supposed to model how disagreement works in science. You examine the data. You articulate uncertainty. You explain why you agree or disagree. You do not wave away evidence with a shrug and a map.
If this is how our professional organizations justify ignoring inconvenient data, then evidence-based medicine becomes a slogan rather than a discipline. And slogans do not protect patients.
The ethical obligation of medicine is not to defend national pride. It is to reduce harm. That obligation does not change at the border.
The correct question is not, “Do we live there?” (though many of us would like to)
The correct question is, “Is the evidence sound, and what can it teach us?”
Anything less is not science. It is ideology in a lab coat.
Reflection / Closing
If we allow geography to substitute for analysis, we abandon the very idea of shared scientific truth. Medicine becomes tribal, defensive, and inward-looking. Patients deserve better than that. So do clinicians. The next time international data challenge our assumptions, we should not ask where it comes from. We should ask whether it is right.


Yes, and.. for some diseases prevalence and exposure risks are connected so some places may have lower rates such that certain health recommendations may be different