Vaginal Progesterone, Revisited: What the New AJOG Meta-analysis Really Shows
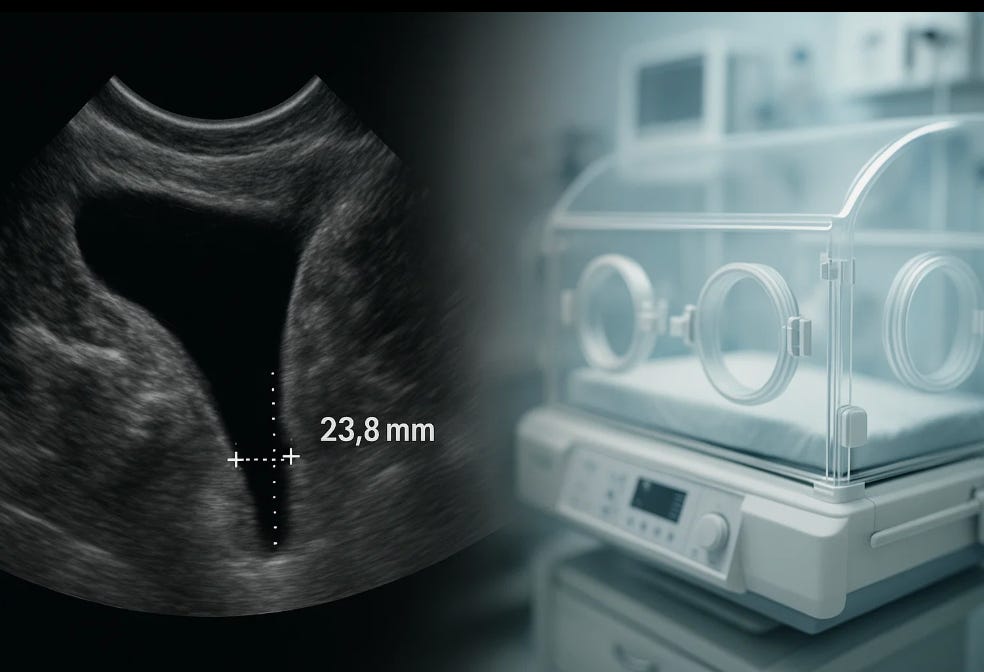
A new individual-patient data meta-analysis cuts through years of controversy and confirms that vaginal progesterone prevents preterm birth in women with a short cervix.
The question of whether vaginal progesterone prevents preterm birth has carried more noise than clarity in recent years. Between PROLONG, shifting guidelines, and widespread clinician uncertainty, many pregnant women with a short cervix have been caught in the middle. The new Research Letter in the American Journal of Obstetrics & Gynecology provides the strongest clarifying evidence to date. It does so by analyzing what matters most: individual patient-level data in women with a sonographic cervical length 25 mm or less and no history of spontaneous preterm birth.
This is the precise population where doubt has been most persistent. And the results are hard to ignore.
What the new AJOG analysis did
The authors performed a subgroup analysis of their recently updated individual patient data (IPD) meta-analysis, restricting the sample to women with:
• A singleton pregnancy
• A mid-trimester transvaginal cervical length ≤25 mm
• No prior spontaneous preterm birth
• Randomized to vaginal progesterone vs placebo across three high-quality trials (n = 686)
The methodology matters. Individual patient-level data corrects for differences in baseline risk, minimizes ecological bias, and allows standardized outcome definitions across studies. This is the highest level of evidence we can reasonably obtain in this domain.
The findings deserve attention
Across all primary and secondary outcomes, the pattern is consistent.
1. Significant reduction in preterm birth <33 weeks
Preterm birth <33 weeks occurred in 11 percent of the progesterone group vs 18 percent of the placebo group (RR 0.65, 95 percent CI 0.45–0.94; P = .02).
A one-third reduction at this gestational age is clinically meaningful. This is the age range where morbidity reduction translates into fewer ventilators, fewer intraventricular hemorrhages, and less long-term neurodevelopmental risk.
2. Consistent benefits across multiple gestational age thresholds
The effect extended across <35, <34, <32, and <30 weeks, with relative risks ranging from 0.61 to 0.70, all statistically significant. The directionality was uniform, even where confidence intervals widened.
This type of coherence across endpoints is what strengthens biological plausibility.
3. Neonatal benefits also reached significance
Infants exposed to vaginal progesterone had significantly lower rates of:
• Respiratory distress syndrome (5 percent vs 9 percent; RR 0.52, 95 percent CI 0.28–0.98)
• Birthweight <1500 g (7 percent vs 13 percent; RR 0.55, 95 percent CI 0.35–0.87)
Other outcomes, including composite neonatal morbidity and mortality, trended in the same favorable direction but did not reach statistical significance. Importantly, nothing moved in the opposite direction.
Why this matters: We are finally seeing signal consistency
The most important contribution of this AJOG study is clarity.
For years, the discourse around progesterone has blurred two distinct clinical questions.
Question 1: Does vaginal progesterone prevent recurrent spontaneous preterm birth in women with a prior preterm birth but a normal cervical length?
Question 2: Does vaginal progesterone prevent preterm birth in women with a short cervix, regardless of their prior history?
The answer to Question 1 has become increasingly uncertain after PROLONG.
The answer to Question 2 has remained consistently supported across multiple meta-analyses, including this new one.
Yet in practice, these two issues have been conflated, leaving many clinicians hesitant to prescribe progesterone even for women with a clearly defined short cervix.
The ethical dimension
When evidence becomes confusing, the ethical risk is that uncertainty translates into inaction. Pregnant women with a short cervix do not have the luxury of time. A median cervical shortening diagnosis occurs between 18 and 24 weeks. Decisions must be made quickly and based on the best available data.
The new AJOG analysis restores that footing.
Failing to offer a therapy that reduces early preterm birth, ventilator days, and very-low-birthweight outcomes when high-quality evidence supports it is, ethically, a different kind of risk: the risk of omission. Pregnant women deserve clarity, not paralysis.
What this means for practice right now
• A sonographic cervical length ≤25 mm in a singleton pregnancy remains a strong indication for vaginal progesterone.
• The benefit applies whether or not there is a prior preterm birth.
• Neonatal benefits strengthen the case for treatment rather than simple observation.
• No evidence suggests harm.
Given this new analysis, arguments that progesterone “might not work” for short cervix are now inconsistent with the totality of patient-level data.
A note about real-world readiness
One strength of the Research Letter is the explicit acknowledgment that multiple international professional societies already recommend vaginal progesterone for this population. The new results confirm those recommendations and provide a clear pathway for clinicians who have been reluctant to commit.
In other words, the field has what it needs. The question now is whether we will use it.
Reflection
Preterm birth is one of the few obstetric complications we can truly prevent in a subset of women with the right intervention at the right time. When the data sharpen, our responsibility sharpens with them. The new AJOG analysis is not just another research update. It is a reminder that progress in obstetrics is often incremental but decisive when viewed through the right lens. The ethical imperative now is to ensure that these findings reach the patients who stand to benefit.