The Evidence Room: “Total” Is Not What You Think
Medical words are supposed to bring clarity. Too often they do the opposite.
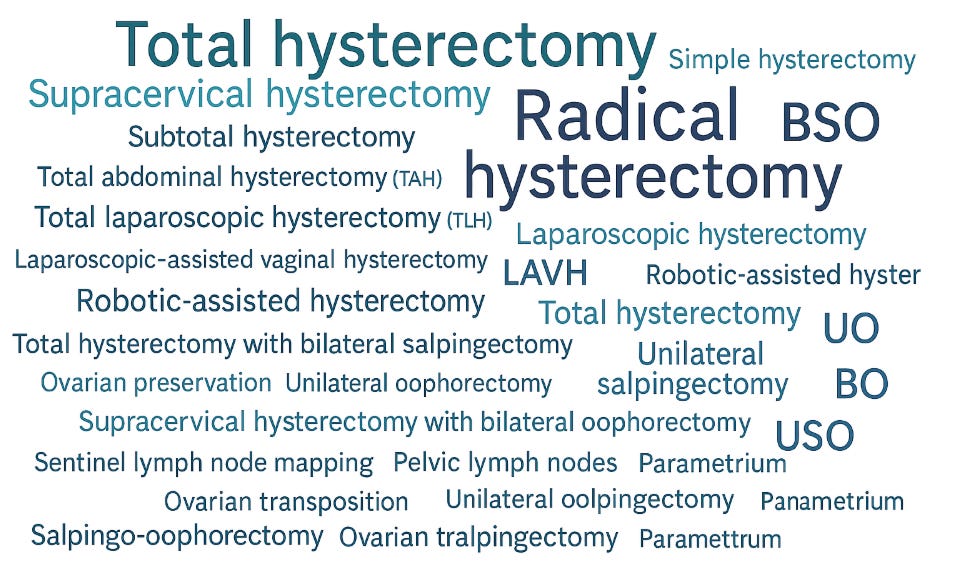
Why Words Count, Yet Often Confuse
Medical words are supposed to bring clarity. Too often they do the opposite. In gynecology, the same term can mean different things to different people. Some words are historical leftovers, some are billing shortcuts, and some are surgical slang that slipped into everyday use.
Patients hear “total,” “complete,” or “radical” and think everything was removed. Surgeons may mean only the uterus and cervix. Electronic records add to the problem when drop-down menus favor quick clicks over precise anatomy. Another trap is mixing route of surgery with what was removed. “Total laparoscopic hysterectomy” describes the approach and that the cervix came out, but it still says nothing about the ovaries or tubes.
Small language mistakes lead to big clinical mistakes. If a cervix was kept, cervical screening must continue. If both ovaries were removed before natural menopause, hormone plans and bone health need attention. If tubes were removed and ovaries saved, cancer risk drops without sudden menopause. Words should map exactly to the body parts involved.
The fix is simple. Name each structure. Uterus. Cervix. Right tube. Left tube. Right ovary. Left ovary. State how the surgery was done. Clear language is part of informed consent, good follow-up, and patient safety.
She was 42, healthy, and scared. “I had a total hysterectomy at 35,” she told me. “So my ovaries were removed for sure. That is what total means.”
It does not. Many patients confuse “total” with “complete.” Neither word tells us whether the ovaries were removed. That detail matters for hormones, long-term health, and future screening. Let’s clear it up.
My Patient
My patient came in with hot flashes and trouble sleeping. She worried she was in menopause and needed hormones. Her chart said “total abdominal hysterectomy.” That term means the uterus and cervix were removed through an abdominal incision. It does not say anything about the ovaries. When we checked her old operative report, I found that her surgeon kept both ovaries. Her symptoms were not due to surgical menopause. Different problem, different plan.
This confusion is common. Words like total, partial, complete, or simple describe the uterus and cervix. They do not automatically include the ovaries. Ovaries are separate. The fallopian tubes are separate too.
Why This Matters
Your ovaries make estrogen, progesterone, and testosterone. Before natural menopause, removing both ovaries causes an immediate hormone drop. That can raise risks for heart disease, bone loss, memory changes, and sexual discomfort. It can also relieve severe endometriosis or prevent ovarian cancer in high-risk patients. The decision is personal and should be informed.
The cervix matters too. If your cervix remains, you may still need cervical cancer screening, depending on your history. If your cervix is removed and your prior Pap tests were normal, you usually do not need further Pap testing. The fallopian tubes matter as well. Removing the tubes while keeping the ovaries can reduce the risk of the most common type of ovarian cancer. Many surgeons now do this when they perform a hysterectomy for benign reasons.
In short, the exact parts removed determine your follow-up care, your hormone options, and your long-term health plan.
The Names, Translated
Here is a plain-language guide you can keep:
Hysterectomy terms about the uterus and cervix
Total hysterectomy: Removal of the uterus and cervix. No information about ovaries or tubes or why it was done
Subtotal hysterectomy (also called supracervical or partial): Removal of the uterus body only, cervix left in place.
Simple hysterectomy: Another term for total hysterectomy when done for benign disease.
Radical hysterectomy: Removal of the uterus, cervix, the upper part of the vagina, and the tissues around the cervix called the parametrium and uterosacral ligaments. Pelvic lymph nodes are usually removed and checked.
Common indications:
Early cervical cancer that has grown beyond a tiny, strictly microscopic area.
Some larger precancerous lesions of the cervix that cannot be safely treated with more limited surgery.
Selected rare cancers that involve the cervix or upper vagina, based on oncology guidance.
Treatment of cervical cancer that recurs after a less extensive procedure, if radiation is not the better option.
Not routine for:
Benign conditions like fibroids, prolapse, or heavy bleeding.
Most uterine or ovarian cancers, which follow different surgical plans.
Do the ovaries come out in a radical hysterectomy:
Not automatically. Radical describes the extent of tissue taken around the cervix and upper vagina. It does not, by itself, include ovaries.
In many premenopausal patients with cervical cancer, the ovaries can be preserved because cervical cancer rarely spreads to them. Sometimes the ovaries are moved up (ovarian transposition) to protect them if radiation might be needed later.
In postmenopausal patients, or if the ovaries look abnormal, the surgeon may remove one or both ovaries and tubes at the same time.
If both ovaries are removed before natural menopause, this causes surgical menopause, which should be discussed in advance, including options for hormone therapy when appropriate.
Approach or route of surgery
Abdominal hysterectomy: Through a larger belly incision.
Vaginal hysterectomy: Through the vagina, no abdominal incisions.
Laparoscopic hysterectomy: Small keyhole incisions with a camera.
Laparoscopic-assisted vaginal hysterectomy (LAVH): Combination of laparoscopy and vaginal surgery.
Total laparoscopic hysterectomy (TLH): Entire operation done laparoscopically.
Robotic-assisted hysterectomy: Laparoscopic surgery using robotic instruments.
Words about the ovaries and tubes
These are separate procedures that may or may not be done with a hysterectomy:
Oophorectomy: Removal of an ovary.
Unilateral oophorectomy: One ovary removed.
Bilateral oophorectomy: Both ovaries removed. This causes surgical menopause if done before natural menopause.
Salpingectomy: Removal of a fallopian tube.
Bilateral salpingectomy: Both tubes removed. Ovaries can be kept.
Salpingo-oophorectomy: Removal of tube and ovary together.
Unilateral salpingo-oophorectomy (USO): One tube and ovary removed.
Bilateral salpingo-oophorectomy (BSO): Both tubes and both ovaries removed.
Opportunistic salpingectomy: Removing both tubes during another pelvic surgery to reduce ovarian cancer risk, while preserving ovaries.
Bottom line: “Total hysterectomy” tells you about the cervix, not the ovaries or tubes.
What Is New or Overlooked
Two changes in thinking are worth knowing:
Fallopian tubes as the origin for many “ovarian” cancers. Many high-grade serous cancers start in the tubes. This is why removing the tubes while keeping the ovaries is increasingly common during benign hysterectomy. It offers cancer risk reduction without instant menopause.
Individualized ovarian decisions. For patients under 45, keeping ovaries can protect heart, bone, and brain health unless there is a strong cancer risk or severe disease like endometriosis that warrants removal. For patients with BRCA or other high-risk syndromes, removing ovaries and tubes at the right age can be lifesaving. One size does not fit all.
Practical Takeaways
For patients and families
Ask these three questions before surgery: Will my cervix be removed. Will my ovaries be removed. Will my tubes be removed.
Get the paperwork. Ask for the operative note and the pathology report. Keep digital copies. The exact words matter.
Know your follow-up.
Cervix removed and past Pap tests normal: you likely do not need Pap tests.
Cervix kept: you still need cervical screening based on routine guidelines.
Understand hormone changes.
Both ovaries removed before natural menopause: talk about menopausal hormone therapy, bone health, and heart risk.
Ovaries kept: you will not have surgical menopause, even if your uterus and cervix were removed.
Cancer risk conversations. If you have a family history of ovarian or breast cancer, ask about genetic counseling before deciding on ovary removal.
For clinicians
Use exact terms in consent and notes. List uterus, cervix, each tube, and each ovary. Avoid “complete” or “total” without details.
Document the route and the rationale. State whether an opportunistic salpingectomy was done and why.
Close the loop. Give patients plain-language discharge instructions that match the actual anatomy removed and the screening plan ahead.
For everyone
Language shapes care. When words blur, follow-up blurs. Accurate names protect patients.
A Relatable Analogy
Think of a house renovation. Saying “we removed the kitchen” tells you the stove and sink are gone. It does not tell you whether the garage was torn down, whether the roof was replaced, or whether the attic was insulated. In pelvic surgery, the uterus is the kitchen. The cervix is the kitchen doorway. The ovaries are the electrical panel for the whole house. The fallopian tubes are a hallway where trouble can start. The work order must list each part. Your health depends on it.
A Quick Glossary You Can Screenshot
Total hysterectomy: uterus plus cervix removed.
Subtotal or supracervical hysterectomy: uterus removed, cervix kept.
Radical hysterectomy: uterus, cervix, nearby tissues removed, usually for cancer.
Route: abdominal, vaginal, laparoscopic, robotic.
Salpingectomy: tube removed.
Oophorectomy: ovary removed.
Salpingo-oophorectomy: tube and ovary removed.
BSO: both tubes and both ovaries removed. Causes surgical menopause if premenopausal.
Opportunistic salpingectomy: both tubes removed, ovaries kept, to lower cancer risk.
What To Do If You Are Not Sure What You Had
Call the surgeon’s office and request the operative note and pathology report.
Look for these phrases: “cervix removed,” “ovaries conserved,” “bilateral salpingectomy,” “BSO,” “subtotal” or “supracervical.”
Share the documents with your current doctor.
Update your medical ID or personal health record so future clinicians see the exact details.
APPENDIX:
All the Names, Expanded
A) Total hysterectomy variants
Uterus and cervix removed. Ovaries and tubes are specified separately.
Total hysterectomy only: Uterus and cervix removed. Tubes and ovaries status not stated.
Total hysterectomy with bilateral salpingectomy: Uterus and cervix removed. Both tubes removed. Ovaries kept.
Abbrev: TAH-BS, TLH-BS, TVH-BS
Total hysterectomy with unilateral salpingectomy: Uterus and cervix removed. One tube removed. Ovaries kept.
Total hysterectomy with BSO: Uterus and cervix removed. Both tubes and both ovaries removed.
Abbrev: TAH-BSO, TLH-BSO, TVH-BSO
Total hysterectomy with USO: Uterus and cervix removed. One tube and the ovary on the same side removed. Opposite ovary and tube kept.
Specify side: with right USO or with left USO
Total hysterectomy with bilateral oophorectomy only: Uterus and cervix removed. Both ovaries removed. Tubes left in place.
Less common today because tubes are usually removed too.
Total hysterectomy with unilateral oophorectomy: Uterus and cervix removed. One ovary removed, the other kept. Tubes status specified separately.
Total hysterectomy with ovarian preservation and ovarian transposition: Uterus and cervix removed. Ovaries kept and moved higher to avoid radiation exposure. Tubes usually removed.
B) Supracervical or subtotal hysterectomy variants
Uterus removed. Cervix kept.
Supracervical hysterectomy only: Uterus removed. Cervix kept. Tubes and ovaries not stated.
Abbrev: SCH
Supracervical hysterectomy with bilateral salpingectomy: Uterus removed. Cervix kept. Both tubes removed. Ovaries kept.
Supracervical hysterectomy with unilateral salpingectomy: Uterus removed. Cervix kept. One tube removed. Ovaries kept.
Supracervical hysterectomy with BSO: Uterus removed. Cervix kept. Both tubes and both ovaries removed.
Supracervical hysterectomy with USO: Uterus removed. Cervix kept. One tube and ovary removed. Opposite ovary and tube kept.
Supracervical hysterectomy with bilateral oophorectomy only: Uterus removed. Cervix kept. Both ovaries removed. Tubes left.
C) Simple hysterectomy variants
“Simple” focuses on uterus and cervix, typically for benign disease. Anatomy combinations mirror “Total.”
Simple hysterectomy only
Simple hysterectomy with bilateral salpingectomy
Simple hysterectomy with BSO
Simple hysterectomy with USO
Simple hysterectomy with unilateral or bilateral oophorectomy
Specify as above for tubes and ovaries.
D) Radical hysterectomy variants
Uterus, cervix, upper vagina, and parametrial tissues removed, often with pelvic nodes. Ovaries are not automatically removed.
Radical hysterectomy only: Ovaries and tubes not specified.
Radical hysterectomy with bilateral salpingectomy: Ovaries kept.
Radical hysterectomy with BSO: Both tubes and ovaries removed.
Radical hysterectomy with USO: One tube and ovary removed.
Radical hysterectomy with ovarian preservation and transposition: Ovaries kept and moved out of the pelvis.
E) Route-specific names that often pair with the above
These describe how the surgery was done. Always add the adnexal details.
Total abdominal hysterectomy (TAH)
Total vaginal hysterectomy (TVH)
Total laparoscopic hysterectomy (TLH)
Laparoscopic-assisted vaginal hysterectomy (LAVH)
Robotic-assisted laparoscopic hysterectomy
Now combine, for example: TLH-BS, TVH-BSO, LAVH with right USO, Robotic radical hysterectomy with ovarian preservation.
F) Focus on tubes and ovaries that commonly accompany hysterectomy
Opportunistic bilateral salpingectomy: Both tubes removed during hysterectomy to lower ovarian cancer risk. Ovaries kept.
Unilateral salpingectomy: One tube removed, often for ectopic or damage.
Bilateral oophorectomy: Both ovaries removed. Causes surgical menopause if premenopausal.
Unilateral oophorectomy: One ovary removed. The other continues hormone production until natural menopause.
USO: One tube and ovary removed on the same side.
BSO: Both tubes and both ovaries removed.
Salpingectomy alone with hysterectomy: Tubes only removed, ovaries preserved.
Salpingo-oophorectomy plus contralateral salpingectomy: For example, left tube and ovary removed, right tube removed, right ovary kept.
G) Common combined phrases you will see in charts
These are highly used in operative notes and discharge summaries.
TAH only
TAH-BS
TAH-BSO
TAH with right USO or TAH with left USO
TLH only, TLH-BS, TLH-BSO, TLH with USO
TVH only, TVH-BS, TVH-BSO
LAVH-BS, LAVH-BSO
Robotic TLH-BS, Robotic TLH-BSO
Radical hysterectomy only
Radical hysterectomy with BS
Radical hysterectomy with BSO
Radical hysterectomy with ovarian preservation
Supracervical hysterectomy only
Supracervical hysterectomy with BS
Supracervical hysterectomy with BSO
Supracervical hysterectomy with USO
H) Less common but important clarifiers
Hysterectomy with bilateral salpingectomy and ovarian conservation: Explicitly states ovaries kept.
Hysterectomy with cystectomy: Ovarian cyst removed. Specify if ovary preserved.
Hysterectomy with adhesiolysis: Scar tissue removed. Still specify tubes and ovaries.
Hysterectomy with sentinel lymph node mapping: Mainly in oncologic cases.
Hysterectomy with ovarian suspension or transposition: Ovaries moved, not removed. State tube status.
I) Quick “read-the-note” recipe
Identify the uterus and cervix plan: total, supracervical, simple, radical.
Identify the tubes: none, unilateral salpingectomy, bilateral salpingectomy.
Identify the ovaries: preserved, unilateral oophorectomy, BSO, USO.
Identify the route: abdominal, vaginal, laparoscopic, robotic.
If oncologic, look for nodes, parametrium, upper vagina, and any ovarian transposition.
J) Abbreviation key you can paste into patient instructions
TAH: Total abdominal hysterectomy
TLH: Total laparoscopic hysterectomy
TVH: Total vaginal hysterectomy
LAVH: Laparoscopic-assisted vaginal hysterectomy
SCH: Supracervical hysterectomy
BS: Bilateral salpingectomy
US: Unilateral salpingectomy
OO: Oophorectomy
UO: Unilateral oophorectomy
BO: Bilateral oophorectomy
USO: Unilateral salpingo-oophorectomy
BSO: Bilateral salpingo-oophorectomy
Key reminder: “Total” tells you the cervix was removed. It does not tell you anything about the tubes or ovaries. Always spell those out.
Ethical Lens
Words are part of informed consent. If a patient hears “total,” and reasonably assumes “everything,” then we failed to communicate. Real consent requires accurate names, clear teaching, and time for questions. That is respect for autonomy in action.
Reflection and Closing
If you have had a hysterectomy, do you know exactly which parts were removed. If you are planning one, do you feel clear on uterus, cervix, tubes, and ovaries. Precision in language leads to precision in care. Ask for the words that match your body. As clinicians, we should give nothing less.