The First Question Nobody Asks at Your Twin Ultrasound
How many placentas there are matters more than how many babies there are. Here is exactly what your monitoring schedule should look like, and why.
You are pregnant with twins. You hear two heartbeats. You see two babies on the screen. You are told congratulations.
What you are almost never told, at least not clearly enough and not early enough, is that twin risk has almost nothing to do with the number of babies. It has everything to do with the placenta.
One Question Changes Everything
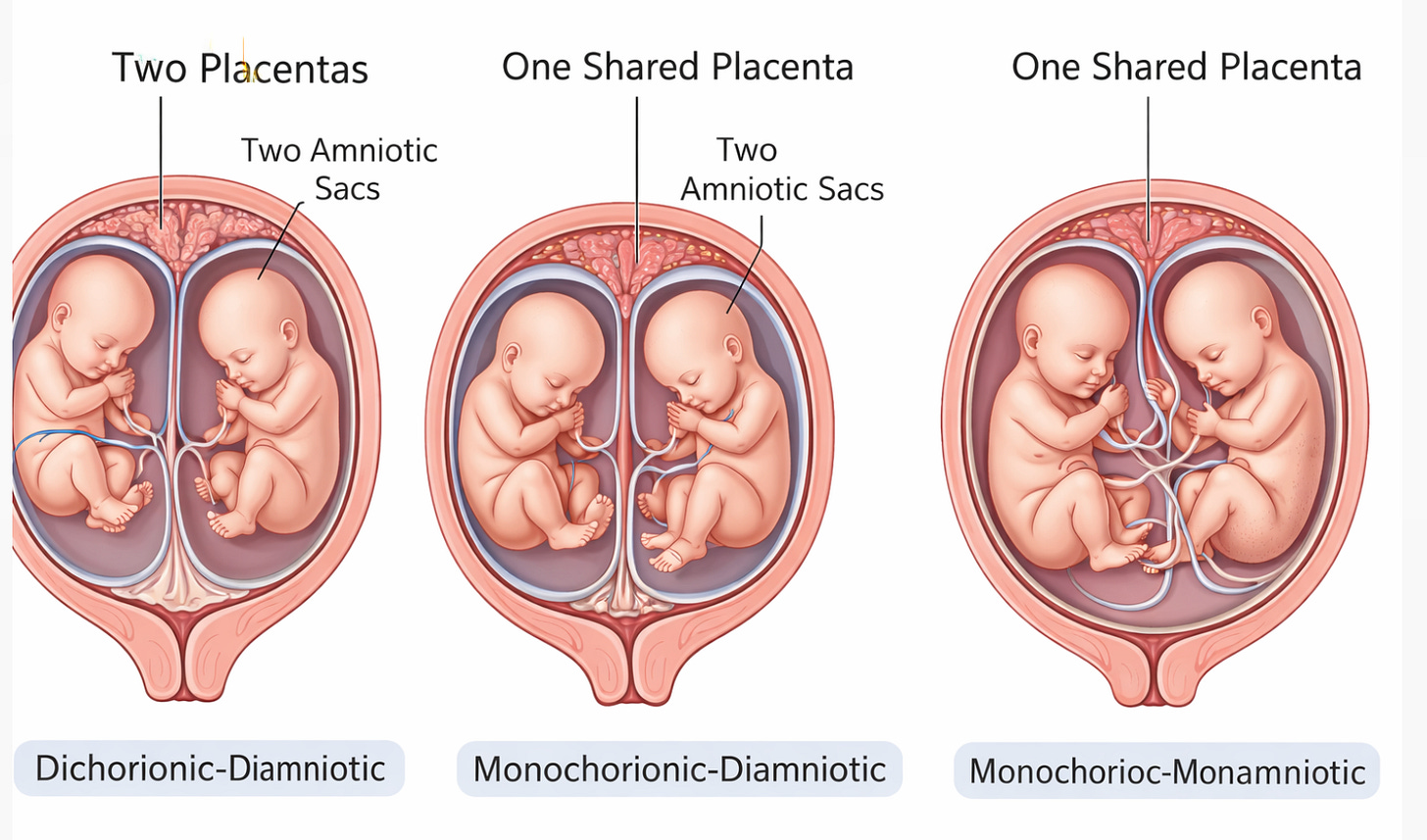
The single most important piece of information in any twin pregnancy is chorionicity: how many placentas are there, and how many amniotic sacs surround the babies?
This is not a detail. It is the foundation of your entire prenatal care plan. It determines how often you are scanned, what your doctors are looking for at each visit, when you will deliver, and what complications can develop between one appointment and the next.
First-trimester ultrasound between 11 and 14 weeks can determine chorionicity with 99.8% accuracy (1). After 14 weeks, that accuracy drops because the membranes between twins become harder to distinguish. A study that confirmed chorionicity by placental pathology or discordant sex in 613 pregnancies found only one misclassification in the entire cohort when the scan was performed in the first trimester (1).
That means there is a narrow window to get this right. If your provider does not determine chorionicity before 14 weeks, you may spend the rest of your pregnancy in the wrong monitoring lane.
Three Types of Twins, Three Different Pregnancies
Twins are classified by biology, not by how many babies there are.
Dichorionic-diamniotic (di-di) twins have two separate placentas and two separate amniotic sacs. This includes virtually all fraternal twins and roughly one-third of identical twins. Because each fetus has its own blood supply, these twins are physiologically independent. The risks are real, including preterm birth, growth differences, and preeclampsia, but they are the lowest-risk twin configuration.
Monochorionic-diamniotic (mono-di) twins share a single placenta but have separate amniotic sacs. This occurs in about two-thirds of identical twins. Because the placenta is shared, blood vessels connect the two fetal circulations. Over 95% of monochorionic placentas have vascular anastomoses linking the twins (2). That single anatomic fact changes everything about how these pregnancies behave. One twin can transfuse blood to the other. One twin can grow while the other falls behind. And the transition from normal to dangerous can happen in days, not weeks.
Monochorionic-monoamniotic (mono-mono) twins share one placenta and one amniotic sac. There is no dividing membrane. The cords can entangle. These pregnancies account for about 1% of all twins and roughly 5% of monochorionic twins (3). Cord entanglement is present in virtually 100% of mono-mono pregnancies when systematically evaluated by ultrasound and color Doppler (4). This is among the highest-risk situations in modern obstetrics.
Why Monitoring Differs by Placental Type
The monitoring schedule for twins is not about doing more ultrasounds. It is about looking for specific complications that are biologically possible only in certain placental configurations. A di-di twin who looks healthy at 24 weeks is unlikely to develop a sudden placental crisis at 26 weeks. A mono-di twin can look completely normal at one visit and show early twin-to-twin transfusion syndrome two weeks later.
This post is part of the “High Risk Pregnancy and Know Your Numbers, Trust Your Body” series. Subscribe to ObGyn Intelligence for the full analysis, including what TTTS looks like, what your monitoring schedule should catch, and the delivery timing numbers you need to bring to your next appointment.