The “Anti-Inflammatory Diet” for (Peri)Menopause: What the Evidence Actually Shows
“Anti-inflammatory diet” isn’t a medical term. There’s no definition in any clinical guideline or textbook. It’s a marketing label applied to whatever foods the author wants to sell you.
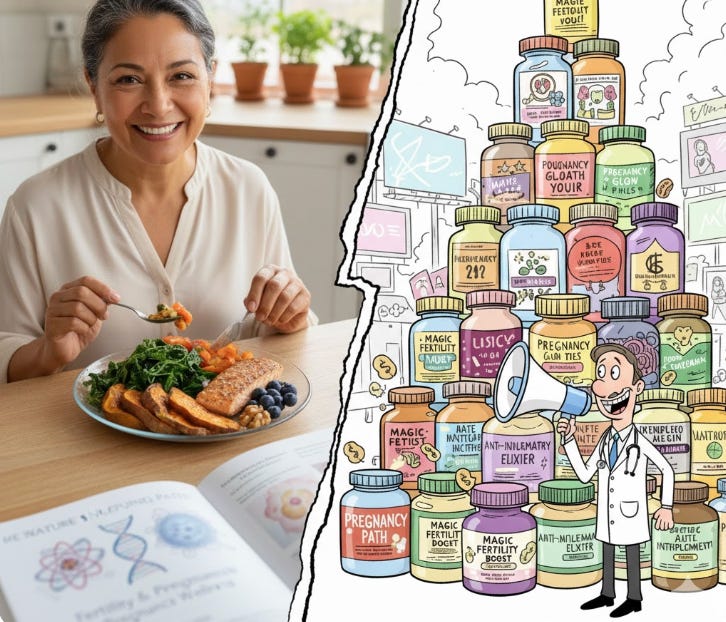
Scroll through any menopause wellness account and you’ll find the same advice: adopt an “anti-inflammatory diet” to ease hot flashes, beat brain fog, and lose that stubborn belly fat. The pitch sounds scientific. Estrogen is anti-inflammatory. When it drops during menopause, inflammation rises. So eat anti-inflammatory foods to fill the gap.
It’s a tidy story. But is it true?
The Problem Starts With the Name
“Anti-inflammatory diet” isn’t a medical term. There’s no definition in any clinical guideline or textbook. It’s a marketing label applied to whatever foods the author wants to sell you—usually some combination of salmon, berries, turmeric, and olive oil, with occasional detours into bone broth and adaptogenic mushrooms.
What does exist is research on the Mediterranean diet, which emphasizes fruits, vegetables, whole grains, fish, and olive oil. Multiple meta-analyses have examined whether this eating pattern reduces inflammatory markers like C-reactive protein (CRP) and interleukin-6 (IL-6).
The findings? Modest reductions in CRP averaging about 1 mg/L. Sounds impressive until you realize the studies show enormous variability (heterogeneity often exceeds 90%), meaning results are wildly inconsistent across trials. Some studies show big effects; others show none. The most recent systematic reviews note that “further high-quality studies will be essential to confirm these findings.”
And here’s the kicker: most of these trials weren’t done in menopausal women specifically. They studied mixed populations, often people with diabetes or heart disease.
What About Hot Flashes?
The best evidence for diet affecting menopausal symptoms comes from trials testing soy—not generic “anti-inflammatory” eating.
A 2021 randomized trial assigned 84 women with frequent hot flashes to either a low-fat vegan diet with half a cup of soybeans daily or no dietary changes. After 12 weeks, moderate-to-severe hot flashes dropped by 88% in the soy group versus 34% in controls. Impressive.
But let’s be clear about what this study tested: phytoestrogens from soy, not “anti-inflammatory” effects. Soy isoflavones are plant compounds that weakly mimic estrogen. They may help hot flashes through estrogen receptors, not by reducing inflammation.
A 2025 meta-analysis of soy isoflavone trials found they were not significantly effective for vasomotor symptoms overall. Some trials showed benefit; others didn’t. The results may depend on whether women can metabolize soy into equol (only about 30% of Westerners can).
In other words: the evidence for soy helping hot flashes is real but inconsistent. The evidence for “anti-inflammatory diets” broadly helping menopause symptoms is much weaker.
The Conflation Game
The wellness industry plays a sleight-of-hand trick here. They take three separate findings:
Mediterranean diet patterns are associated with lower inflammatory markers in some studies
Soy phytoestrogens may reduce hot flashes in some women
Healthier eating patterns are associated with better overall health
Then they blend these into one magical concept—the “anti-inflammatory diet for menopause”—as if the mechanisms are the same. They’re not.
Eating more vegetables and less processed food is sensible advice for everyone. Saying that specific foods “fight inflammation” to cure your hot flashes goes beyond what the science supports.
What Actually Works
For hot flashes, hormone therapy remains the most effective treatment for women who can safely use it. If you prefer dietary approaches, trying soy foods (tofu, edamame, soy milk) for 2-3 months is reasonable—about 50% of women in trials get meaningful relief.
For general health during menopause, a Mediterranean-style eating pattern makes sense—not because it’s “anti-inflammatory” but because it’s associated with lower cardiovascular risk, better blood sugar control, and possibly better bone health. These are things menopausal women actually need.
The Bottom Line
When you see “anti-inflammatory diet for menopause,” translate it as: “eat vegetables and fish, which is fine advice dressed up in sciency language.”
The inflammation story isn’t entirely wrong—estrogen loss does increase inflammatory markers. But the leap from “inflammation increases” to “eating turmeric will fix your menopause” is marketing, not medicine.
Your grandmother’s advice to eat your vegetables didn’t need a mechanism. It doesn’t need one now either.


Excellent breakdown of how marketing terms get conflated with medical evidence. The point about 90% heterogeneity in the Mediterranean diet studies is critical, people overlook that variation means the effect size is unreliable across populations. I've seen the same pattern in other wellness claims whre individual trials get spun into universal recommendations. The distinction between phytoestrogen mechanisms and inflammation reduction is especially important.