Should Pregnant Patients Consider Adding Hereditary Cancer Screening to Routine Prenatal Genetic Testing?
What is regular genetic screening in pregnancy?
When someone becomes pregnant, one of the standard conversations in prenatal care is about carrier screening. This testing looks at whether a parent carries genetic changes (mutations) that could affect the baby if both partners carry the same condition. Common examples include cystic fibrosis, spinal muscular atrophy, and certain blood disorders. Carrier screening is focused on the health of the baby, not the long-term health of the pregnant patient.
Why think beyond the baby?
Pregnancy is often the first time many patients undergo genetic testing and counseling. It’s also a unique opportunity to look at the mother’s own health risks—particularly the risk for inherited cancers such as breast, ovarian, colon, and uterine cancers. This is where hereditary cancer screening comes in.
What is hereditary cancer screening?
This testing looks for gene mutations like BRCA1/2 (linked to breast and ovarian cancer) or Lynch syndrome (linked to colon and uterine cancer). Identifying these risks early can guide not just pregnancy decisions, but also future screening and prevention for the patient herself and her family.
Why combine them?
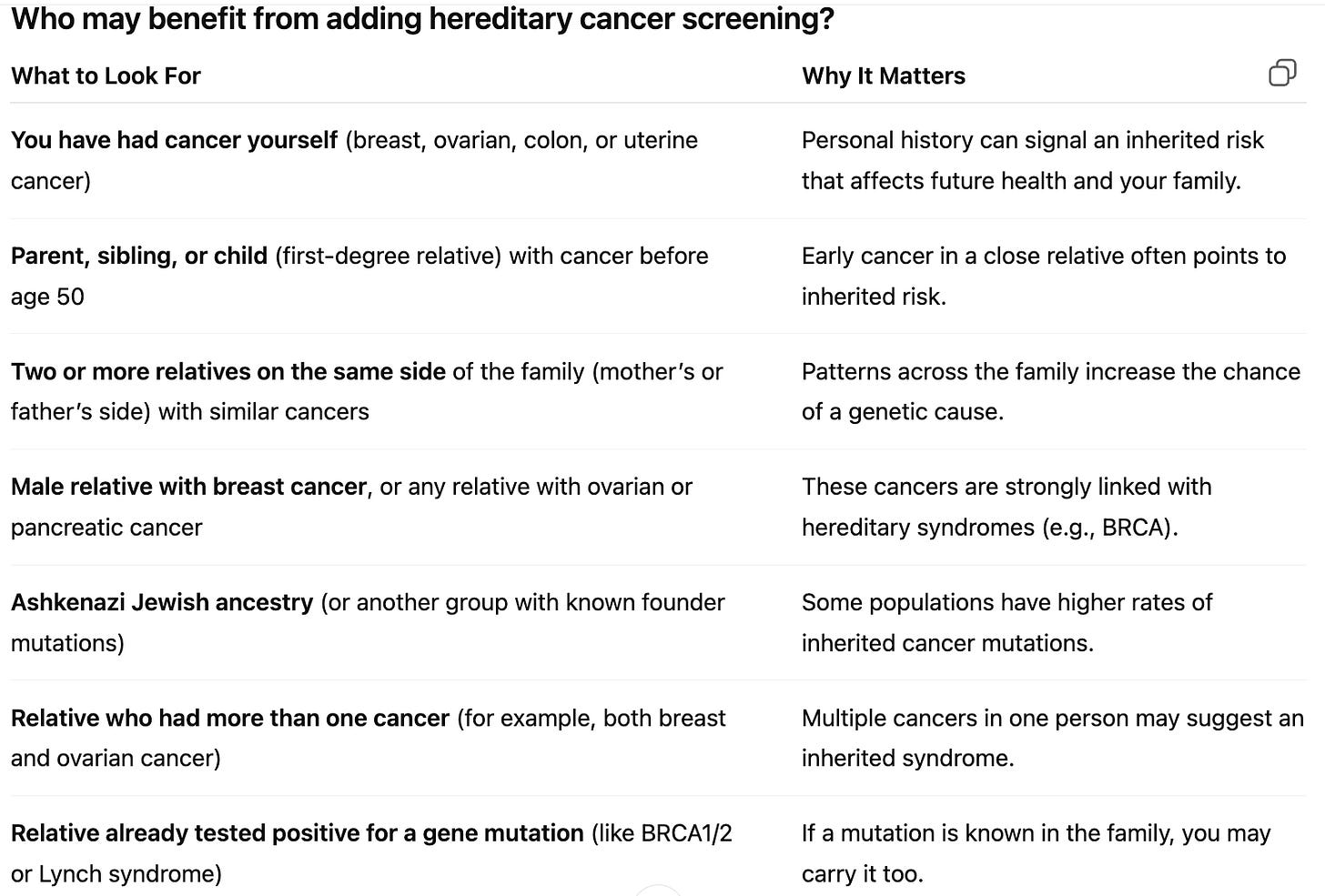
Convenience: One appointment, one sample, broader answers.
Efficiency: Reduces duplicate testing and missed opportunities.
Family health: Results can benefit not only the baby but also the patient and relatives.
Prevention: Detecting hereditary cancer risk allows proactive steps—earlier screening, tailored medical decisions, and sometimes life-saving prevention.