“Not What I Expected” Is the Most Honest Outcome Measure in Home Birth
When stories replace data, preventable harm gets reframed as “birth trauma.”
This essay responds to a public Reddit thread in which parents who planned home births describe outcomes that sharply diverged from what they were told to expect. And it also responds to reports of women dying at home births in Ireland and Australia.
Across dozens of first-person accounts, writers recount delayed recognition of complications, urgent hospital transfers, neonatal injury, maternal hemorrhage, infection, and lasting emotional distress. Many describe having been reassured that their pregnancies were “low risk,” only to realize after the fact that the limits of home birth care and the realities of obstetric emergencies were never clearly disclosed. Read together, the thread functions less as a collection of anecdotes and more as a collective after-action report on a system that fails in predictable ways.
I have done extensive research on home births in the US and published extensively on the many adverse outcomes including a recent study in January 2026 which reported that US home birth midwives hide their bad outcomes but failing to legally report bad outcomes..
Opening
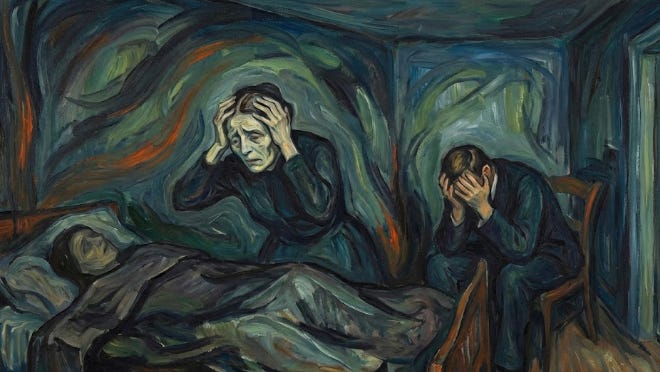
Home birth advocacy often promises empowerment, control, and physiologic normalcy. The lived experiences collected in “Not What I Expected” tell a very different story. These are not rare edge cases. They are narratives of delayed transfers, dismissed warning signs, neonatal compromise, and parents left to process harm after being assured that everything was “low risk.” Reading them as an obstetrician and ethicist, the common thread is not bad luck. It is predictable systems failure.
What the stories actually show
Across the accounts, several patterns recur. Labor complications escalate without timely escalation of care. Fetal distress is normalized or reframed. Prolonged labors continue far beyond evidence-based thresholds. When transfer finally occurs, it is late, chaotic, and adversarial. Parents describe shock at how quickly a “normal” labor became an emergency, and how little preparation they had been given for that possibility. These are not failures of individual intention. They are failures of setting, standards, and accountability.
Risk is not eliminated by selection
A central claim of home birth advocacy is careful risk selection. The narratives undermine that claim. Postpartum hemorrhage, shoulder dystocia, neonatal depression, infection, and hypertensive complications occur in patients who were labeled “low risk” until the moment they were not. Obstetrics is defined by low-frequency, high-impact events. Hospitals exist not because birth is usually dangerous, but because when danger arises, seconds and minutes matter. A setting that cannot provide immediate operative delivery, blood products, neonatal resuscitation, and multidisciplinary response is structurally unprepared for obstetric reality.
Normalization of delay
One of the most concerning themes is the normalization of delay.
Prolonged rupture of membranes, hours of abnormal fetal heart tones by intermittent auscultation, rising maternal fever, and failure to progress are repeatedly minimized. Delay is reframed as patience. Concern is reframed as fear-based medicine.
By the time transfer occurs, the window for prevention has often closed. This is not shared decision-making. It is information asymmetry combined with ideology.
Informed consent without material disclosure
True informed consent requires disclosure of material risks, including the limits of the setting itself. Many storytellers describe learning only afterward that cesarean delivery, neonatal intensive care, or rapid transfusion were never available options at home. Consent that omits foreseeable emergencies is ethically incomplete. Autonomy is not respected when patients are reassured rather than informed, or when worst-case scenarios are dismissed as “hospital bias.”
Accountability gaps
When outcomes are poor, responsibility becomes diffuse. There is no morbidity and mortality conference. No mandatory reporting system with clinical granularity. No licensure standards comparable to hospital-based obstetrics. Parents describe being left alone to reconcile grief with narratives that the outcome was unavoidable or spiritually meaningful. In any other domain of health care, repeated adverse outcomes without corrective action would trigger oversight. Home birth too often operates outside that basic safety loop.
The false comparison to other countries
Advocates frequently invoke countries where home birth is integrated. The stories here reflect a different reality. In those systems, home birth is embedded within regulated midwifery, strict selection criteria, mandatory transfer protocols, seamless hospital integration, and real consequences when standards are violated. Cherry-picking the outcome while ignoring the infrastructure is intellectually dishonest. You cannot import the reassurance without importing the rules.
What patients actually needed
Reading these accounts, what parents wanted was not maximal intervention. They wanted honesty. They wanted early recognition of trouble. They wanted timely transfer without conflict. They wanted professionals who understood that safety is not the enemy of dignity. None of that is incompatible with respectful obstetric care. It is incompatible only with settings that cannot deliver it.
There are other stories online of home births that went wrong:
Closing reflection
The most striking phrase in these narratives is not medical. It is moral: “I didn’t know.” When harm follows reassurance, the ethical failure is upstream. Birth settings should be judged not by ideology or anecdotes, but by how they perform when things go wrong. Stories like these should not be dismissed as outliers. They are warning signals. The responsible response is not defensiveness, but reform, standards, and the courage to say that some risks cannot be ethically offered in the name of choice alone.


One thing I've noticed is the commodification of hospital birth and birth-trauma narratives on social media. Individuals do not assess risk solely on population-level probabilities or the types of statistics we provide in our office or in inpatient counseling, but often through powerful, emotional narratives they view online. Vivid stories, particularly those involving harm (real or perceived), amplify risk and make rare events feel common and imminent. And narratives where there is a villain, be it a nurse, doctor (or both), and a savior, doula/homebirth midwife, are *very* easy to understand. It's practically Little-Red-Riding-Hood-easy. Add the "upvoting" of trauma, and it can be a competition to see who had the worst in-hospital birth versus the most wow-factor home birth. I have seen this in discussion boards, where someone says, "It's not a true free-birth unless you are 100% alone, like, your husband can't even be there." These narratives are shaped by social contagion.
Women giving birth 100 years ago, when maternal death was 1 in 125 and infant death nearly 1 in 10, tragic stories would be shared in communities of perhaps 10 to 15 individuals. Today, a single influencer’s account may reach millions, making them a disproportionate authority. Fear becomes socially reinforced, risk is decontextualized, and individual stories are recast as prescriptive truth, with profound consequences for how women understand and navigate childbirth risk. Add to all of this a healthcare workforce that may be limited in time, staffing, and facility capacity. The issue is complex, to be sure, but one must not ignore the income and social clout women earn and put in their pockets when their stories of hospital birth are vilified and home birth valorized.
The point that you can’t use Canadian statistics for US outcomes is critical. I’d like to see regulation and integration of home birth services so US women who desire home birth can achieve those excellent outcomes. Home birth can be safe when part of a regulated (and non adversarial) system.