Is Denmark Irresponsible For Not Recommending Hepatitis B Vaccines Routinely To Newborn Babies
Despite omitting universal infant hepatitis B and routine varicella vaccination, Denmark consistently achieves low rates of vaccine-preventable disease, lower infant mortality than the United States.
U.S. medical organizations have repeatedly criticized Denmark for maintaining a shorter childhood vaccine schedule than the United States, often implying that fewer routine vaccines reflect lower standards or increased risk.
That criticism misunderstands how public health policy actually functions in a high-performing, tightly integrated health system. Denmark bases vaccine recommendations on population-level disease prevalence, near-universal prenatal screening, and reliable follow-up care, rather than on a one-size-fits-all approach.
Despite omitting universal infant hepatitis B and routine varicella vaccination, Denmark consistently achieves low rates of vaccine-preventable disease, lower infant mortality than the United States, and strong maternal-child health outcomes. In other words, Denmark is not underperforming or taking reckless shortcuts. It is applying a different risk-management strategy that aligns with its epidemiology and health system capacity, and the outcomes show that the system is functioning effectively.
Infant Mortality Rate (United States vs Denmark)
United States: approximately 5.3–5.5 deaths per 1,000 live births in the most recent data (2024 estimate). MacroTrends
Denmark: approximately 3.0–3.4 deaths per 1,000 live births in the most recent data (2023–2025 range).
Interpretation in simple terms
Babies in the United States die before age one at a rate roughly 1.5–1.8 times higher than in Denmark. This means for every 1,000 babies born alive, about 5.3 to 5.5 in the U.S. die before one year of age, whereas in Denmark only about 3.0 to 3.4 do.
These differences persist even when accounting for variations in reporting definitions and methods across countries. Health System Tracker
The disparity reflects broader differences in healthcare access, social determinants, and maternal-child health systems rather than a simple function of vaccination schedules alone.
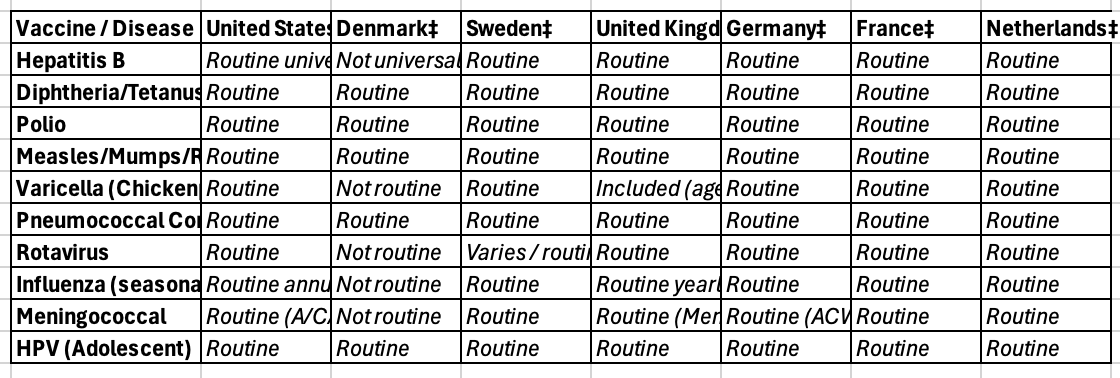
Newborn/Infant Vaccine Comparisons
† The CDC in 2025 recommended childhood immunization against approximately 16–18 diseases, though a recent advisory vote changed universal hepatitis B timing and broad recommendations are under review, drawing criticism from U.S. public health experts who emphasize differences in disease burden between countries. Reuters+1
‡ Denmark historically recommends fewer vaccines than the U.S., excluding routine childhood vaccination for hepatitis B, hepatitis A, rotavirus, varicella, influenza, RSV, and meningococcal disease for all children. STAT Sweden generally follows broader EU vaccine schedules including varicella and influenza. National immunization schedules in Nordic countries vary but include core childhood vaccines such as MMR, DTP, polio, and PCV. nhwstat - nordic health & welfare National schedules for the UK (Green Book), Germany (STIKO), France, and the Netherlands all include core vaccines (DTP, polio, MMR, PCV, HPV) with some variation in adolescent and optional vaccines. Wikipedia
Limitations and caveats. Direct comparison is constrained by differences in age group recommendations, risk-based vs universal policies, and evolving schedules. Some European countries do not universally recommend certain vaccines (e.g., Denmark for rotavirus or influenza) because of different epidemiology or health system structure. The U.S. schedule is among the most comprehensive globally and any proposed reductions have been widely criticized by pediatric and infectious disease professionals.
Why Denmark is an outlier in vaccine policy
Denmark does not include universal hepatitis B vaccination for all infants or routine varicella vaccination for all children because its public health authorities rely on comprehensive prenatal screening and very low disease prevalence in the general population to target prevention. Denmark screens nearly all pregnant women for hepatitis B and only vaccinates infants born to mothers who test positive, with high follow-up and prevention of mother-to-child transmission. This targeted strategy differs from the former universal birth-dose hepatitis B vaccination and routine varicella vaccination used for decades in the United States. The UK, Sweden, Germany, France, and the Netherlands generally include hepatitis B and varicella vaccines in their universal schedules (with some age/timing variations) because those countries operate with different epidemiological data and public health frameworks.†
Hepatitis B prevalence among pregnant women (current best estimates)
United States: The prevalence of chronic hepatitis B infection among pregnant women is estimated at approximately 0.7% to 0.9%. This reflects a combination of U.S. population diversity and incomplete prenatal screening in some regions.†
Denmark: Among pregnant women tested in comprehensive screening programs, hepatitis B surface antigen positivity is approximately 0.26% overall, with very low prevalence (≈0.012%) among women of Danish origin and higher rates in subgroups born in endemic regions.†
What this means in everyday terms
In absolute numbers, more pregnant women in the United States carry hepatitis B than in Denmark, which reflects both higher prevalence overall (due to migration patterns and heterogeneous populations) and less uniform access to prenatal care and screening.
Denmark’s strategy depends on near-universal screening and effective follow-up, which works well in that healthcare system with low hepatitis B prevalence, but may not be directly transferable to larger, more diverse populations where screening coverage is uneven.