Investigate Before We Indict - PART 3: When “Preventable” Becomes a Weapon
How maternal mortality statistics are misunderstood and misused
Series introduction
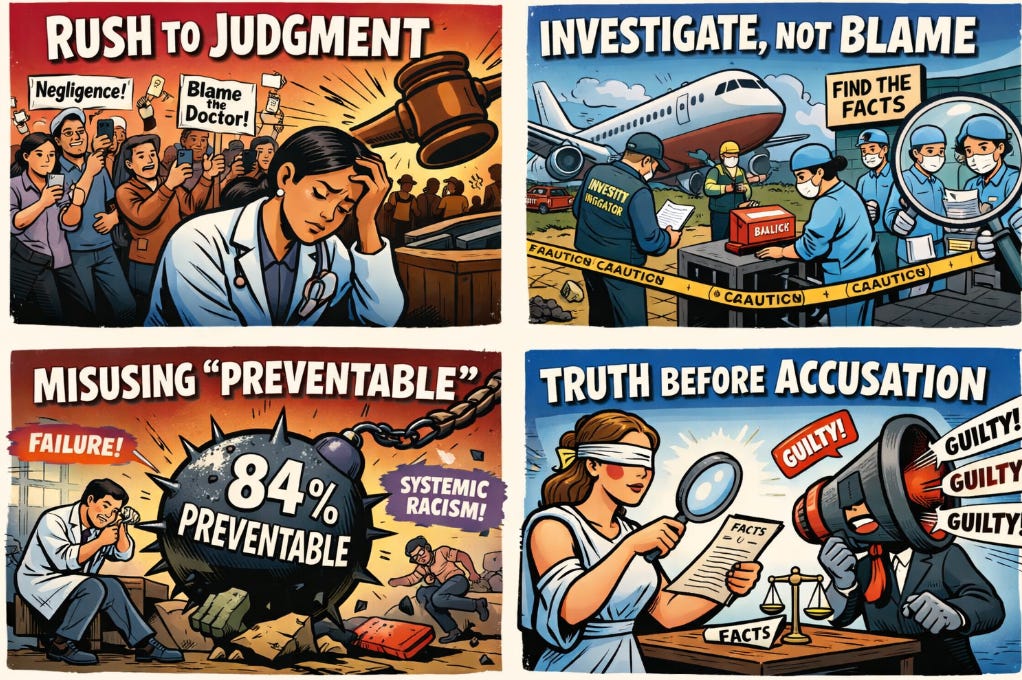
This essay is Part 3 of a four-part Obstetric Intelligence series titled Investigate Before We Indict. Part 1 examined the rush to judgment that follows maternal death. Part 2 explored why abandoning disciplined investigation undermines safety. Part 3 turns to data, focusing on how the term “preventable” in maternal mortality statistics is widely misunderstood and routinely weaponized. Part 4 will conclude by examining what clinicians, organizations, and advocates owe the truth when tragedy becomes public.
1. What the CDC Actually Means by “Preventable”
One statistic dominates public discussion of maternal mortality: approximately 84 percent of pregnancy-related deaths in the United States are described as “preventable.” The number is real. The meaning most people attach to it is not.
Maternal Mortality Review Committees use a deliberately broad definition of preventability. A death is classified as preventable if reviewers believe there was at least some chance that an intervention might have altered the outcome. “Some chance” is sufficient. The intervention can occur at multiple levels, including patient behavior, community resources, provider actions, facility capacity, or broader system factors.
This framework is designed for quality improvement, not for fault-finding. It asks a retrospective question: can we imagine a counterfactual world in which something, somewhere, might have been different? If the answer is yes, the death is labeled preventable.
That is a useful exercise for prevention planning. It is not a judgment about the quality of care delivered in a specific case.
The distinction matters because the word “preventable” carries moral weight. Outside technical review circles, it is widely understood to mean that someone failed, that negligence occurred, or that the system broke down. That inference is understandable. It is also incorrect.
2. Preventability Is Not Negligence
A woman who receives timely, guideline-concordant obstetric care and dies from peripartum cardiomyopathy may still be classified as having experienced a preventable death if reviewers believe earlier recognition or different screening might have helped. A woman who dies after an amniotic fluid embolism may also fall into this category. So may a woman murdered by an intimate partner if better screening, social support, or community interventions might have changed the outcome.
In none of these cases does the classification establish that the clinician failed, that care was substandard, or that racism operated at the bedside. The designation reflects counterfactual reasoning, not culpability.
Yet in public discourse, the nuance disappears. “Preventable” is treated as synonymous with “caused by failure.” The statistic becomes a moral indictment rather than a quality improvement signal.
This conflation is not merely semantic. It reshapes how deaths are reported, how clinicians are portrayed, and how policy priorities are set. It encourages immediate blame rather than careful analysis. It substitutes accusation for understanding.
Importantly, the CDC’s framework does not disentangle social determinants from clinical care. Housing instability, transportation barriers, insurance gaps, chronic disease burden, and community violence are all embedded in preventability assessments. To collapse these complex, upstream factors into claims about obstetric care quality is a category error.
3. The Ecological Fallacy in Real Time
Population-level maternal mortality statistics reveal real and unacceptable disparities. Black women in the United States die at substantially higher rates than White women. Structural racism shapes health long before pregnancy begins. These are established facts.
What population-level data cannot do is explain individual deaths.
Inferring that a specific maternal death was caused by racism, negligence, or system failure because such factors operate at the population level is a classic ecological fallacy. It attributes group-level associations to individual cases without evidence.
This error is now occurring in real time, amplified by social media and advocacy narratives. Individual tragedies are immediately framed as exemplars of systemic failure, often before any facts are known. Investigation becomes secondary to message.
The consequences are serious. Clinicians are publicly accused without evidence. Institutions are condemned without review. Families are offered certainty where only uncertainty exists. Most damaging of all, the credibility of equity-focused reform is weakened when claims outrun data.
Equity efforts depend on precision. They require distinguishing between failures of care and failures of social structure. When those distinctions are blurred, resources are misdirected and trust erodes.
If every death is framed as proof of the same explanation, even when investigation later shows otherwise, skepticism grows. Legitimate concerns are dismissed as ideological rather than empirical.
Preventability statistics were never meant to adjudicate guilt. They were meant to prompt humility, reflection, and improvement. When they are weaponized, they do the opposite.
If we care about maternal safety and equity, we must insist on disciplined interpretation. Data should guide inquiry, not replace it. And statistics should never substitute for investigation.