Post Summary (629 upvotes) Five days postpartum, a mother describes a 48-hour induction that ended in emergency cesarean. Foley balloon caused immediate severe contractions with no pain management offered. Pitocin started the next day with bed confinement for monitoring. Epidural failed.
She developed chorioamnionitis with fever, contractions every 30 seconds, vomiting. At full dilation, baby’s head was malpositioned and too large; fetal distress led to emergency C-section. Too weak to hold her baby after delivery. Hospital prohibited overnight visitors, leaving her to care for newborn alone post-surgery. Now being told to “be grateful” for a healthy baby while she cries reliving the experience.
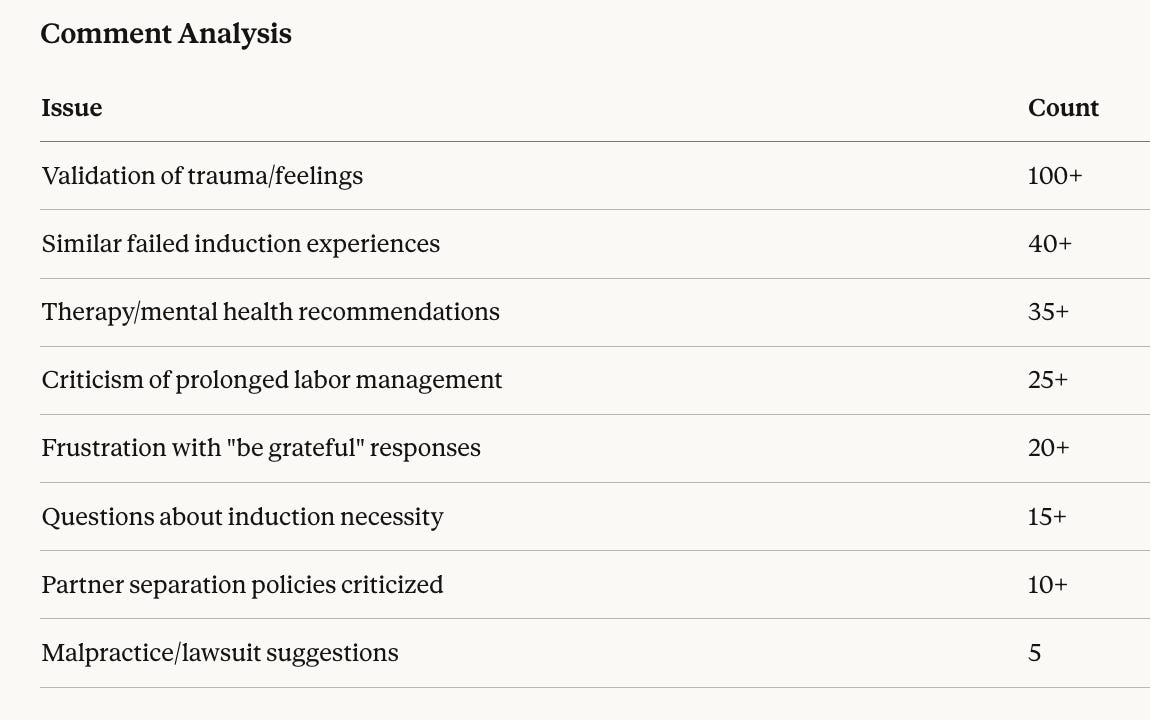
Comment Summary (242 comments)
Overwhelmingly validating. Commenters shared similar traumatic experiences, recommended trauma-focused therapy (EMDR mentioned repeatedly), and expressed frustration with the “healthy baby” dismissal. Multiple Australian commenters identified the no-overnight-visitor policy as typical of their system, connecting to Australia’s recent parliamentary inquiry into birth trauma.
Comment
The recurring phrase "at least you have a healthy baby" reveals obstetric culture's fundamental failure: reducing maternal care to a single outcome metric while dismissing the patient who achieved it. A woman who develops sepsis, endures failed anesthesia, undergoes emergency surgery, and is left alone to care for a newborn is not "healthy" by any reasonable definition. The medical system produced two survivors but left one traumatized. Professional responsibility requires acknowledging that how we deliver care matters as much as whether the baby survives.