"abortion": When a Word Impedes Proper Medical Care
Why we need new language for medically indicated procedures in obstetric emergencies
Over the past several years, anti-abortion laws across the United States have collapsed the entire spectrum of obstetric care into a single politicized term. These laws rarely distinguish between an elective termination and the urgent, medically indicated procedures required to treat hemorrhage, infection, previable rupture of membranes, severe preeclampsia, or lethal fetal anomalies. By forcing clinicians to document these emergencies under the same label, legislators have transformed a political category into a clinical barrier. Physicians are left practicing in an atmosphere of legal uncertainty, and pregnant women in emergencies face delays while hospitals, lawyers, and administrators debate terminology rather than physiology. This is more than a language problem. It is a patient safety problem created by statute. And it killls women.
The word “abortion” is used today for a wide range of clinical situations, yet it is the wrong word for many of them. In obstetrics, we treat emergencies where a pregnant woman’s life, fertility, or health is in immediate danger. We treat fetal conditions that cannot be reversed.
These are medical situations that require clear thinking and accurate language. The problem is that our public vocabulary has not kept up with clinical reality. The result is confusion at best and life-threatening delays at worst.
Many women who are told they need a procedure for hemorrhage, infection, ruptured membranes before viability, severe preeclampsia, fatal fetal anomalies or even ectopic pregnancies are told they are having an “abortion.” That term is politically charged. It is not medically precise. It places clinicians and patients inside an ideological frame that has nothing to do with the emergency in front of them. The point of medicine is to treat the patient’s condition. The point of language is to make that treatment possible.
Across the United States, legal statutes written by nonclinical actors now decide which words appear in medical records. As a result, many physicians must document an emergency intervention as an “abortion” even when the intent is not pregnancy termination but saving a woman’s life. This creates a collision between legal terminology and clinical accuracy. It also creates risk. When the wrong word is used, hesitation grows. When hesitation grows, care becomes dangerous.
We have already seen the consequences. Obstetricians in several states report that hospital counsel and risk officers now ask whether a medically indicated procedure meets the legal definition of “abortion” rather than the clinical definition of emergency intervention. That shift slows decision making. A woman with ruptured membranes at 17 weeks and developing sepsis needs immediate care. A woman with severe preeclampsia at 22 weeks and rising liver enzymes needs immediate care. A fetus without kidneys cannot survive. These are facts. They are not political debates.
Language shapes how quickly a clinician can act. If the only term allowed is “abortion,” some physicians will pause, worry about prosecution, or wait for documentation. These delays can kill. They can also cause permanent morbidity, including future infertility. I have practiced long enough to remember when our field focused on clarity first and politics never. Today, the political narrative is intruding on the exam room. It is doing so through a single word.
Clinical Precision Matters
Medicine depends on precise definitions. When we use the wrong term, we distort the clinical picture. A woman with chorioamnionitis does not need an “abortion.” She needs urgent evacuation of an infected uterus to prevent sepsis. A woman with severe-range blood pressures and end-organ symptoms does not need an “abortion.” She needs expedited delivery to prevent stroke or liver rupture. A fetus with anencephaly does not have a survivable condition. The intervention is management of a nonviable pregnancy. These distinctions are not semantic. They guide triage, consent, and risk communication.
How One Word Creates Ethical Distortion
Ethics begins with truthful communication. When laws force clinicians to use inaccurate terminology, informed consent becomes compromised. A woman may believe she is being asked to “choose an abortion” when in reality the alternative is infection, hemorrhage, or death. Mislabeling shifts moral weight onto a patient who did not ask for the emergency. It assigns intent where there is none. Ethical practice requires neutral language that reflects the actual medical purpose. Without this clarity, respect for autonomy cannot be achieved.
Consequences for Safety and Timeliness
Delays in obstetric emergencies are dangerous. They raise maternal morbidity. They increase ICU admissions. They place fertility at risk. When clinicians must call legal, ethics, or administration before treating predictable complications such as PPROM with infection or severe preeclampsia, time is lost. In some cases, these delays have resulted in worsening sepsis, loss of future fertility, or emergency hysterectomy. The language is directly affecting the outcome. Safety cannot coexist with forced ambiguity.
What Better Language Looks Like
We already have the tools to fix this. Obstetrics has a long tradition of descriptive, neutral terminology. Instead of “abortion,” we should document medically indicated delivery, treatment of previable PPROM with infection, management of nonviable pregnancy, evacuation for hemorrhage control, or delivery for maternal stabilization. These phrases describe clinical intent honestly. They create clarity for patients, clinicians, auditors, and courts. They also restore respect for the woman experiencing the emergency.
Reclaiming Professional Authority
Language in medicine should be set by clinicians. It should be anchored in physiology, pathology, and the real needs of the woman sitting in front of us. Legislatures, advocacy groups, and political movements do not manage obstetric emergencies. Physicians do. It is time for our professional societies to lead by defining a modern, clinically accurate vocabulary for these situations. If we do not reclaim that authority, someone else will. And the consequences will continue to fall on pregnant women and the clinicians who care for them.
Therapeutic/Indicated Termination of Pregnancy (TTP) for [Indication]
Why it is better: While it still uses the root “termination,” the modifier “therapeutic” or “indicated” strictly categorizes the procedure as a medical treatment for a disease state, distinct from elective procedures.
Medically Indicated Delivery
Why it is better: This reframes the event as a labor and delivery process. It is accurate for second-trimester interventions (e.g., for severe preeclampsia) where the fetus is delivered but cannot survive, emphasizing that the management is obstetric in nature.
Here are 10 important medical indications for pregnancy termination (uterine evacuation) categorized by when they typically present or become critical in the first versus the second trimester.
First Trimester (Early Pregnancy)
These conditions often present an immediate threat to the mother’s life due to hemorrhage, infection, or the inability of the maternal cardiovascular system to adapt to early pregnancy physiology.
Ectopic Pregnancy Implantation of the embryo outside the uterus (e.g., fallopian tube) is a non-viable pregnancy that carries a high risk of rupture and catastrophic hemorrhage. The text notes that “abortive outcomes” such as ectopic pregnancy are distinct events often excluded from standard delivery definitions but represent critical intervention points.
Septic Abortion / Early Sepsis Infection in the uterus, sometimes following an incomplete miscarriage, can rapidly progress to septic shock. Sepsis is a leading direct obstetric cause of death and a severe maternal morbidity indicator.
Severe Cardiac Decompensation (Early Onset) For women with significant pre-existing cardiac disease (e.g., pulmonary hypertension), the early hemodynamic changes of pregnancy can precipitate heart failure. Cardiovascular disease accounts for nearly one-quarter of maternal deaths.
Hyperemesis Gravidarum with End-Organ Damage While not explicitly detailed as a mortality cause in the text, severe cases leading to “acute renal failure” (an SMM indicator) or severe electrolyte imbalance fall under the category of serious maternal medical conditions.
Second Trimester (Pre-Viability)
These indications often involve complications that arise as the pregnancy advances, such as placental issues, hypertensive disorders, or the diagnosis of fetal anomalies.
Preterm Premature Rupture of Membranes (PPROM) Rupture of the amniotic sac before viability leaves the fetus with little chance of survival and exposes the mother to high risks of intrauterine infection. The text explicitly cites PPROM as a complication where denial of abortion forces women to continue pregnancies at significant risk.
Severe Preeclampsia / Eclampsia The onset of severe hypertensive disorders with end-organ damage (seizure, stroke risk) before viability is a definitive indication for delivery to prevent maternal death. “Hypertensive disorders of pregnancy” are a leading cause of mortality and eclampsia carries a low but specific weighted mortality risk.
Lethal Fetal Anomalies Conditions diagnosed via anatomy scan (e.g., anencephaly, renal agenesis) where the fetus cannot survive outside the womb. The text notes that denial of abortion in these cases forces women to carry non-viable pregnancies to term, increasing their risk profile without benefit.
Chorioamnionitis (Intra-Amniotic Infection) Infection of the membranes and amniotic fluid, often following PPROM, can lead to maternal sepsis. Infection is a leading contributor to pregnancy-related mortality.
Placental Abruption / Massive Hemorrhage Premature separation of the placenta causing uncontrollable bleeding. Hemorrhage is a dominant cause of maternal death and “obstetric hemorrhage” protocols are cited as key to preventability.
Peripartum Cardiomyopathy / Heart Failure This condition often presents later but can manifest in the second trimester. Heart failure/arrest is a top weighted SMM indicator with a mortality risk of over 22% when present. Continuing the pregnancy places a potentially lethal strain on the compromised heart.
ACOG does not have a single, consolidated “checklist” of medical indications for termination. (Maybe they should?)
In fact, ACOG has explicitly argued against creating such a list.
In response to state abortion bans and legal questions regarding “medical emergencies,” ACOG released guidance stating that “it is impossible to create an inclusive list of conditions that qualify as medical emergencies.” Their stance is that clinical situations are complex and nuanced, and attempting to legislate via a static list would inevitably fail to capture every life-threatening scenario, potentially tying a physician’s hands in a crisis.
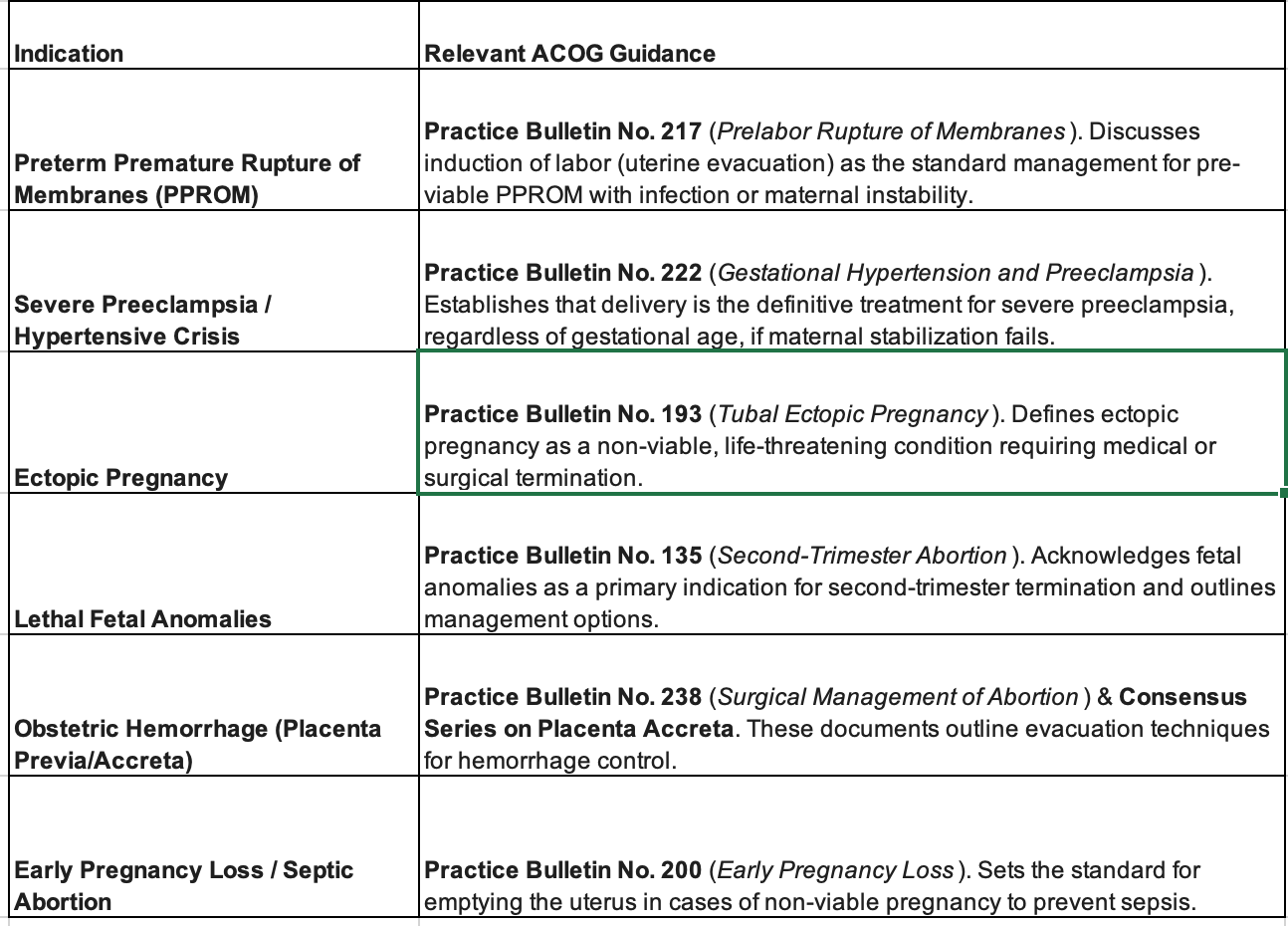
However, while they do not have a single “master list,” they do publish specific clinical guidelines (Practice Bulletins and Committee Opinions) that establish the standard of care for the conditions you requested.
Here is how the conditions from your previous list map to ACOG’s official clinical guidance:
ACOG Clinical Guidance for Specific Indications
Summary of ACOG’s Stance
Clinical Judgment over Checklists: ACOG maintains that a physician’s judgment is necessary to determine when a condition has become life-threatening, rather than waiting for a patient to meet specific criteria on a legislative list.
“Medical Necessity” Statement: ACOG has issued Statements for the Record (e.g., to congressional committees) explicitly listing conditions like placental abruption, bleeding from placenta previa, preeclampsia, and cardiac or renal conditions as examples where abortion may be “the only measure to preserve a woman’s health or save her life,” but these are illustrative examples, not an exhaustive list.
The ethical question is direct. Will we allow a single politicized word to delay emergency care and endanger pregnant women? We already have. Or will we restore accuracy by naming these procedures for what they are: essential medical treatments provided in moments when clarity saves lives?


The linguistic precision argument here is really important. When politicized terminology overrides clinical descriptors, it creates hesitation at exactly the wrong moments. The peripartum cardiomyopathy example stands out because it demonstrates how broad the spectrum of emergency indications really is, going way beyond what most legislators probablyimagine when crafting these laws. I remember a case discussion where a patient with severe cardiac dysfunction was stuck in documentation limbo while legal teams debated language, and valuable time got wasted. The proposed alternative terms like "medically indicated delivery" or "therapeutic TTP" seem cleaner and would likely reduce the administrative friction tht slows emergency response.
Thank you for addressing an important issue. A woman who has tragically experienced loss of ability to carry her pregnancy to term needs compassion and care, rather than be called by derogatory terms such as habitual aborter, or a train wreck. A doctor examining his patient who is in the process of losing her third pregnancy, saying, "You can kiss this one goodbye", with a dangling cigar from his lips. Saying, "you can do it again", after he examined an unfortunate patient who lost not once, or thrice, but 24 times. Another one, "why do you want to get pregnant, you are too old, (fertility expert telling the woman who not only had difficulty getting pregnant at 34 but has miscarried 4 times. These are some of many derogatory, inappropriate interactions voiced by unfortunate patients seeking help with their problems in pregnancy. "Doctors acting like a premadonna and treating us, his patients, like dirt".