A new Lancet publication shows over 20-times missing Apgar scores in US home births
Evidence before this study
We searched PubMed and Google Scholar from inception to June 1, 2025, for peer-reviewed studies published in English using the search terms “home birth”, “birth center”, “out-of-hospital birth”, “Apgar score”, “missing data”, “neonatal mortality”, and “informative missingness”. Existing research has established that planned home births in the United States are associated with higher rates of adverse neonatal outcomes compared with hospital births. However, comparative safety studies often rely on datasets where Apgar scores are assumed to be missing at random. Previous studies have noted the presence of missing data in birth certificate registries but have not systematically quantified whether this missingness differs by birth setting or modeled its potential to bias safety estimates. There is a lack of large-scale population-based analyses examining the “informative missingness” of Apgar scores specifically in the context of US birth settings.
Added value of this study
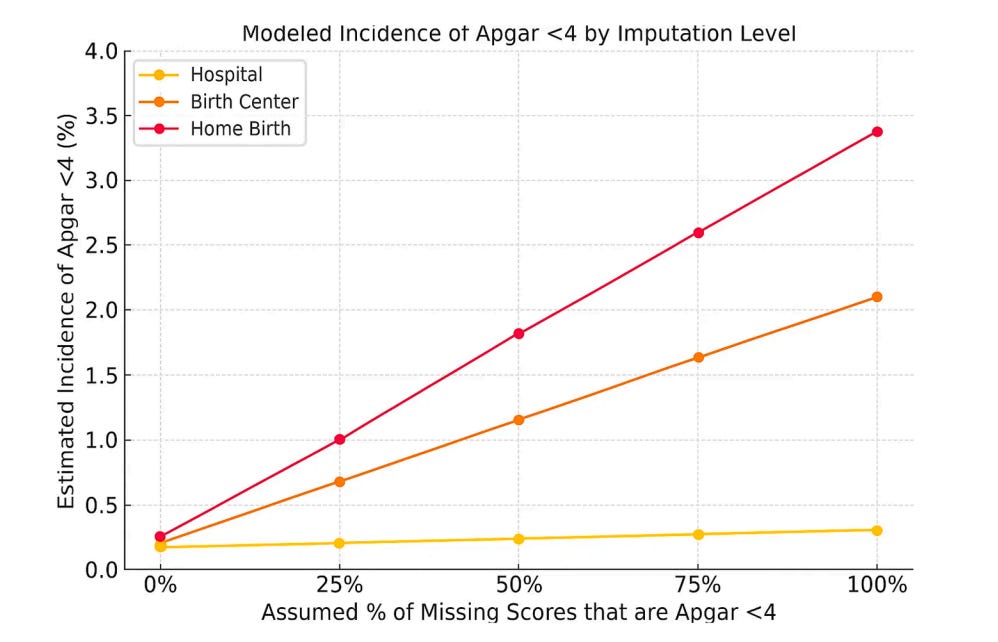
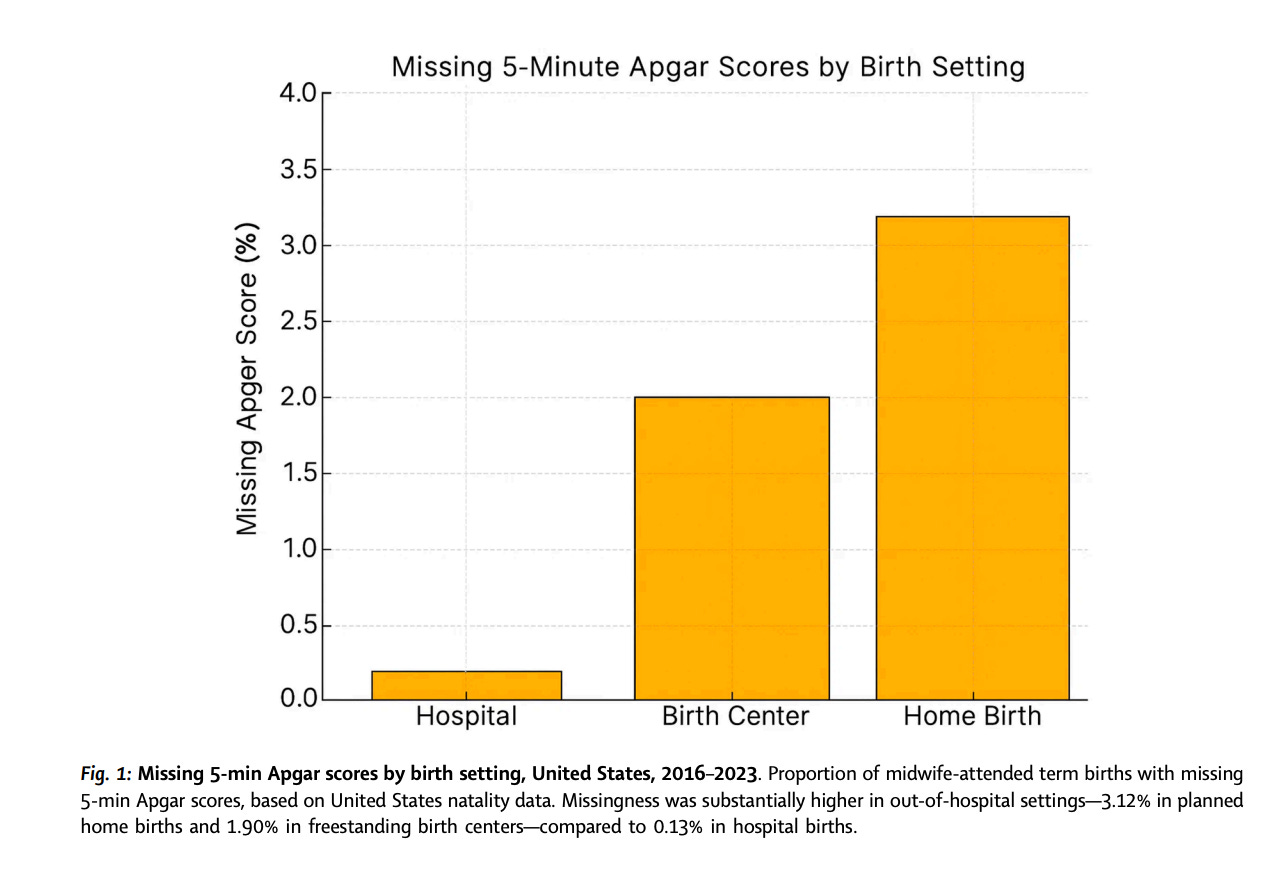
To our knowledge, this is the first population-based study to systematically analyze the pattern and impact of missing 5-min Apgar scores across US birth settings (hospital, freestanding birth center, and planned home birth) using a dataset of over 3 million midwife-attended births. We identified a substantial disparity in data completeness: 5-min Apgar scores were missing 24-fold more frequently in planned home births compared to hospital births. Using deterministic sensitivity analysis, we demonstrated that even modest assumptions about these missing scores representing adverse outcomes (informative missingness) significantly increase the estimated relative risk of severe neonatal compromise in out-of-hospital settings. This study provides a new methodological framework for evaluating birth safety data that accounts for systematic non-reporting.
Implications of all the available evidence
The systematic non-reporting of Apgar scores in out-of-hospital settings compromises the validity of current safety comparisons and undermines informed consent. Evidence suggesting “equivalent safety” for home births may be biased by the exclusion of adverse outcomes that are selectively not recorded. Regulatory bodies should enforce mandatory reporting of neonatal outcomes across all birth settings to ensure data integrity. Future research on birth setting safety must incorporate sensitivity analyses to account for non-random missing data, and clinical counseling for families considering home birth should include transparency about the limitations of current safety data.